Over 40% of clinics that launched RPM in the last two years either paused or discontinued it within the first six months, according to a 2024 American Medical Group Association survey.
The most common reasons were staff burden, low patient engagement, and unclear reimbursement returns.
At CandiHealth, we’ve seen these pain points up close, and solved them. In this blog, we’ll break down why some clinics drop out of RPM after six months, what signs indicate risk, and how your clinic can avoid the same pattern using CandiHealth Remote Patient Monitoring platform.
Our RPM model eliminates Wi-Fi and app dependencies through preconfigured cellular devices, provides consistent data on a centralized dashboard, and simplifies billing with a flat monthly fee.
By removing technical friction and administrative load, we help clinics focus on consistent monitoring, patient engagement, and measurable outcomes that sustain RPM beyond the six-month mark.
Why Do Some Clinics Drop Out of RPM After 6 Months?
The early months of a Remote Patient Monitoring (RPM) program often bring optimism. Clinics start strong—patients are enrolled, devices are distributed, and reimbursements begin to flow. But as months pass, enthusiasm gives way to operational strain. By month six, many clinics start facing RPM program fatigue, and several pause or shut down entirely.
Below are the most common RPM challenges that lead clinics to discontinue their programs:
- Workflow inefficiencies and staff burnout.
- Low patient engagement and adherence
- Reimbursement delays and billing errors
- Technology and integration issues.
- Lack of measurable ROI
- Insufficient training and unrealistic expectations
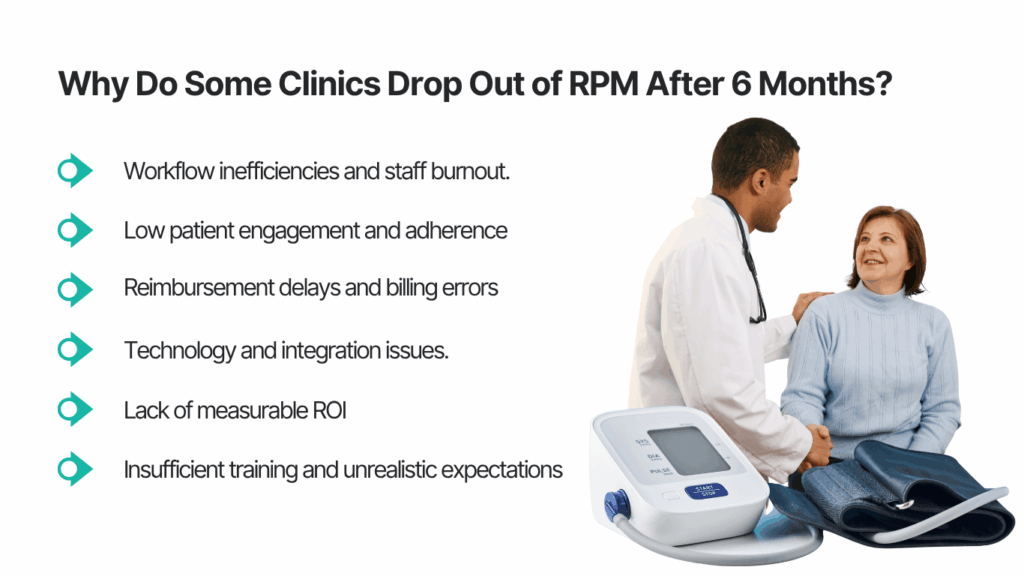
Here is the breakdown of most common challenges faced by RPM clinics.
1. Workflow and Staffing Challenges
RPM adds new daily responsibilities—reviewing alerts, calling patients, documenting care, and submitting claims. Without a defined workflow or dedicated staff, these tasks pile up. The result is staff burnout and inconsistent patient follow-ups.
2. Low Patient Engagement
Even the best RPM setup fails if patients don’t stay consistent. Some forget to take readings; others stop responding to check-ins. Over time, low participation rates make it hard to show measurable outcomes, weakening the program’s perceived value.
3. Reimbursement and Administrative Complexity
RPM billing requires detailed documentation for codes like CPT 99453–99458. Missing data, incomplete time logs, or unverified readings can lead to denied claims or delayed payments. When revenue lags, clinics start questioning the effort-to-return ratio.
4. Technology and Integration Issues
Device pairing errors, Wi-Fi dependencies, and lack of EHR integration often disrupt the data flow. Technical glitches not only frustrate staff but also discourage patients, leading to lower compliance and missed insights.
5. Lack of Clear ROI
RPM takes time to show clinical and financial results. If a clinic expects instant impact such as higher reimbursements or better outcomes, they may lose patience before reaching the proof stage.
6. Unrealistic Expectations and Limited Training
Many clinics underestimate what’s needed to sustain RPM long term. Without proper onboarding, performance tracking, or guidance, the team may feel unprepared to handle alerts, educate patients, or manage billing efficiently.
In short, most RPM dropouts happen because clinics struggle to balance technology, workflows, and patient engagement at once. Sustained success depends on early setup, staff training, consistent monitoring, and supportive technology—something CandiHealth’s simplified, cellular RPM model directly addresses.
How CandiHealth Solves Common RPM Problems
Here’s how CandiHealth helps clinics overcome the biggest challenges that typically cause RPM programs to fail after six months:
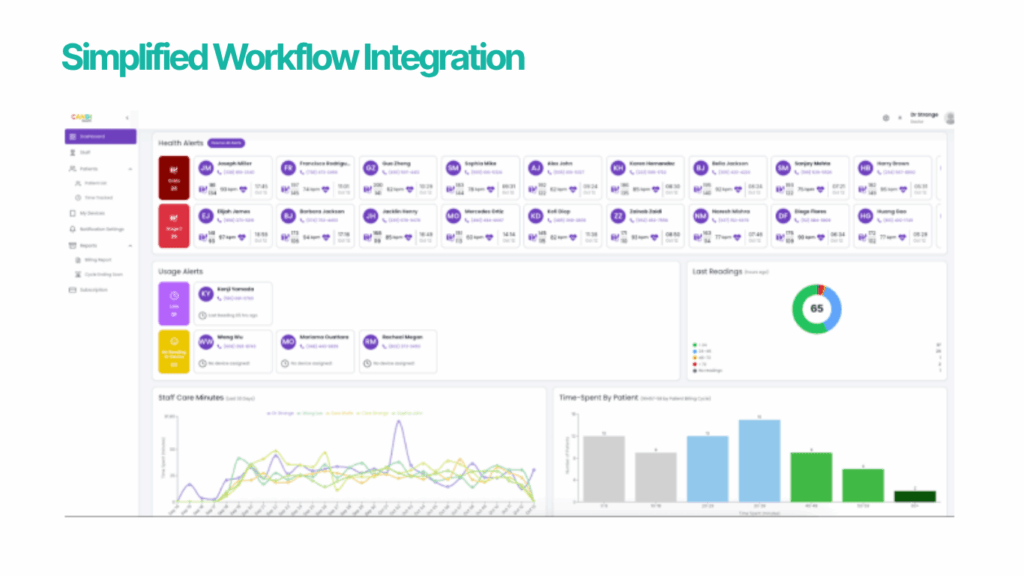
1. Simplified Workflow Integration
CandiHealth removes extra steps from your care team’s day. Our devices automatically uploads readings to a centralized clinical dashboard, organizes patients by status, and flags abnormal results in real time.
No manual tracking, no daily spreadsheet updates. This helps clinics cut admin time and maintain a consistent RPM workflow without overburdening staff.
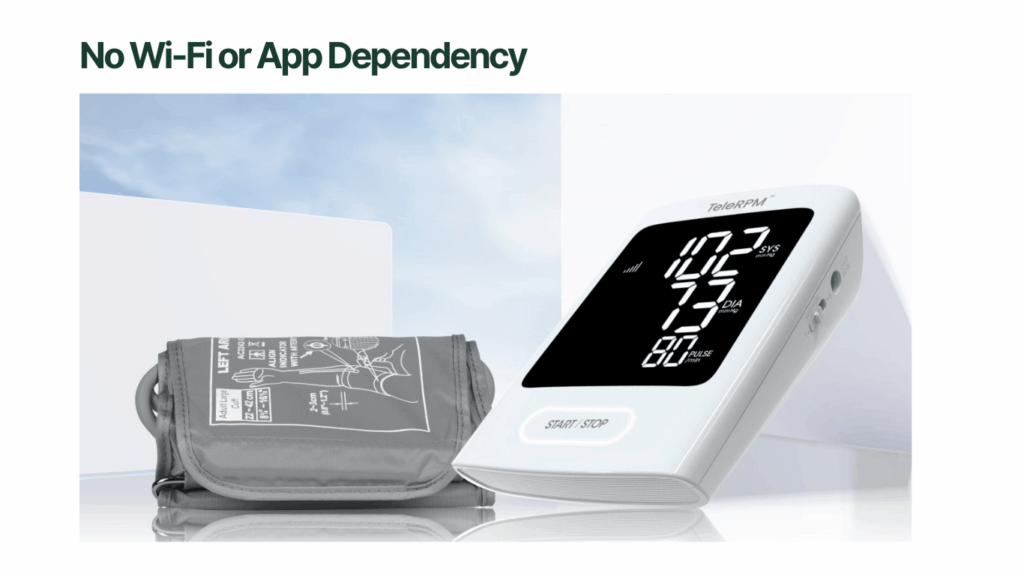
2. No Wi-Fi or App Dependency
Most RPM programs fail when patients can’t connect their devices or lose Wi-Fi access. CandiHealth uses preconfigured cellular devices that transmit data automatically.
Patients don’t need smartphones, apps, or internet access, making compliance easier for elderly or rural populations. This single change often improves patient adherence by over 70%.
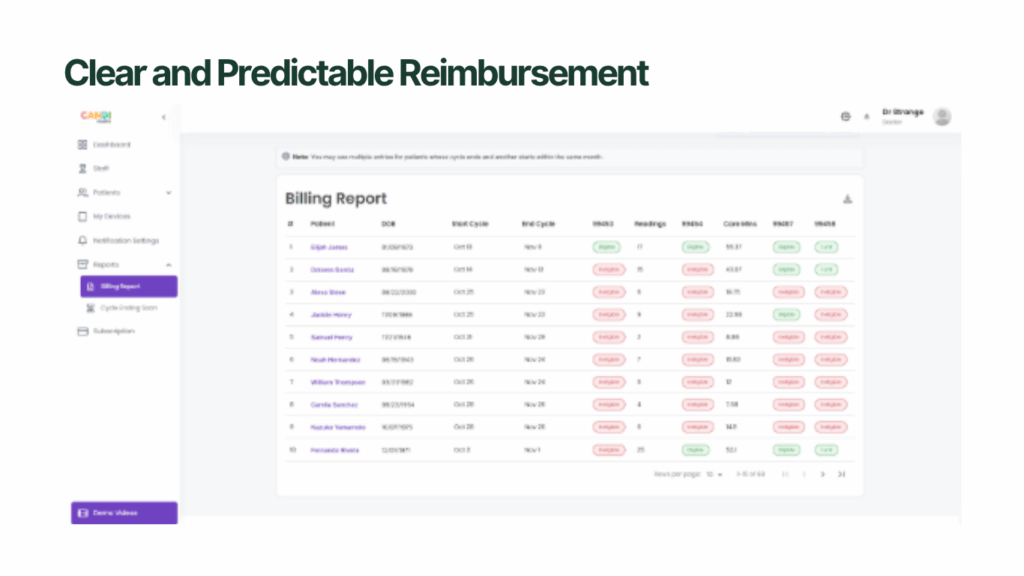
3. Clear and Predictable Reimbursement
Many clinics give up when revenue doesn’t match effort. With CandiHealth’s flat monthly pricing model, there are no hidden platform fees or per-reading charges.
Clinics can easily calculate net RPM revenue from codes like 99453-99458 and plan ROI upfront using our revenue calculator. This transparency makes RPM financially sustainable long term.
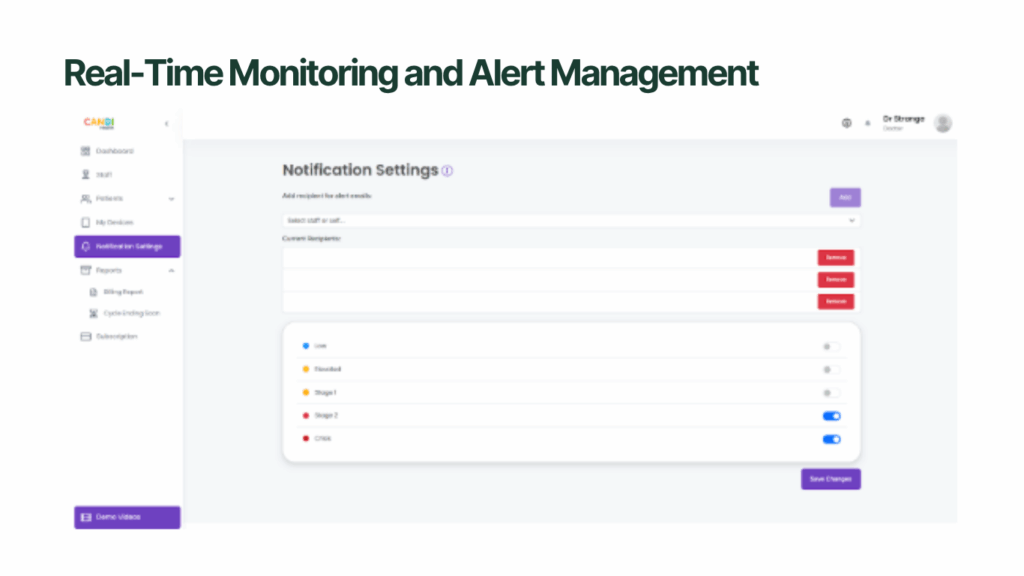
4. Real-Time Monitoring and Alert Management
RPM fatigue often comes from alert overload. CandiHealth solves this through smart triage — flagging only high-risk readings that need attention. This ensures care teams spend time where it matters most, improving both efficiency and patient safety.
Most RPM programs fail not because the idea is flawed — but because execution is hard. CandiHealth bridges that gap by combining simple cellular devices, real-time monitoring, and predictable pricing into one streamlined system. Clinics that partner with CandiHealth don’t just start RPM — they sustain it.
Clinic Success Story: From Dropout Risk to Sustainable RPM
When X Primary Care, a mid-sized clinic in Texas, launched its RPM program, the staff expected quick results. Within the first three months, they enrolled 55 patients with hypertension and heart failure using Bluetooth BP devices. But by month four, readings became inconsistent, claims were delayed, and the nursing team felt overwhelmed managing alerts manually.
By the sixth month, only half of their enrolled patients were still transmitting data. The clinic’s management was ready to pause the program, until they decided to switch to CandiHealth’s cellular RPM system.
What Changed After the Switch:
- Patient Adherence Improved: The preconfigured cellular BP devices started sending readings automatically, even from areas with no Wi-Fi. Within six weeks, daily transmission rates rose from 54% to 88%.
- Staff Efficiency Increased: The centralized dashboard sorted alerts by risk, allowing nurses to focus only on critical cases. They saved nearly 5 hours a week previously spent on manual tracking.
- Billing Became Predictable: Using CandiHealth’s flat-fee model and built-in revenue calculator, the clinic projected earnings for CPT codes 99453–99458 with accuracy and avoided unexpected platform costs.
- Patient Feedback Improved: Patients reported feeling “more connected” to their care team because readings were automatically reviewed and followed up on.
Within three months of using CandiHealth, clinic not only stabilized its RPM program but expanded it to include diabetic patients. The clinic’s leadership described the transition as “a relief — it finally feels manageable.”
Key Takeaway
RPM success doesn’t depend on luck — it depends on simplicity, automation, and support. When clinics remove technical and administrative friction, participation goes up, staff stress goes down, and financial sustainability follows.
CandiHealth’s cellular-based system helps clinics achieve exactly that — turning short-lived pilots into long-term, data-driven care programs.
Conclusion: Making RPM Sustainable
Clinics drop out of Remote Patient Monitoring because it becomes complicated to manage. When daily workflows, billing, and patient engagement fall out of sync, even good programs lose momentum.
CandiHealth helps clinics stay consistent by removing those barriers. With cellular devices that connect automatically, clear flat-rate pricing, and built-in support, your team can focus on care instead of technical issues or billing stress.
If your clinic is ready to sustain RPM beyond the six-month mark, visit CandiHealth to see how a simpler approach keeps both staff and patients engaged for the long term.
Frequently Asked Questions (FAQs)
1. Why do clinics stop their remote patient monitoring (RPM) programs after six months?
Clinics often stop RPM because workflow demands exceed expectations: staff time increases, patient engagement drops, and reimbursement delays emerge. When the effort outweighs visible outcomes within the first six months, many clinics decide to pause or discontinue their programs.
2. What key metrics should a clinic track to keep an RPM program from failing?
Track these metrics early and regularly:
- Percentage of eligible patients enrolled
- Device adherence (% of days with valid data
- Staff time per patient per month
- Billing claim approval rate and reimbursement lag
- Number of alerts generated vs. actioned
- Early clinical trend improvements (e.g., blood pressure, weight)
Monitoring these helps catch risk of dropout early.
3. Can staffing and technology issues really cause an RPM program to fail?
Yes. When devices require Wi-Fi, apps, or multiple steps, patients struggle. When staff lack workflows or are overloaded reviewing alerts and documentation, burnout sets in. These combined tech and staffing burdens are among the top causes of RPM program drop-out.
4. How long does it take for a clinic to see results from an RPM program?
Most clinics begin to observe meaningful results within 4 to 6 months providing patient adherence is strong and workflows are established. Early wins (device use, alerts triaged, reimbursement flowing) help maintain momentum and reduce the risk of program drop-out.
5. What role does reimbursement complexity play in RPM program retention?
Reimbursement complexity plays a major role. Programs using codes such as CPT 99453–99458 require correct documentation and time logs. Delayed or denied claims reduce confidence. When clinics cannot clearly forecast revenue or months pass without payment, they are far more likely to discontinue the program.