Table of Contents
Carolyn doesn’t look sick.
But she manages hypertension, early-stage diabetes, and struggles with mobility. Her clinic is a 40-minute drive. Some weeks, she skips appointments, not because she’s careless, but because it’s exhausting.
Multiply Carolyn by millions, and you begin to see the mounting pressure on both patients and providers.
According to the CDC, six in ten U.S. adults live with at least one chronic disease, and four in ten have two or more. These conditions require regular monitoring, yet the traditional, appointment-based model can’t handle this kind of ongoing demand.
That’s where Remote Patient Monitoring (RPM) comes in. It doesn’t replace in-person care, instead, it complements it by keeping the connection going in between visits.
In the sections ahead, we’ll explore how RPM fits into real care settings and why it’s becoming a quiet essential in chronic care management.
What is Remote Patient Monitoring (RPM)?
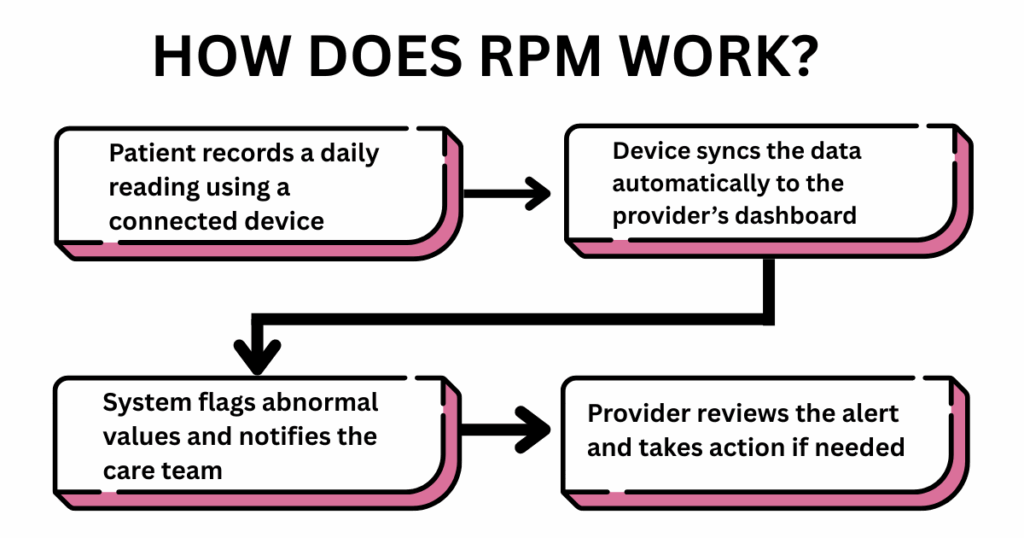
Remote Patient Monitoring (RPM) allows providers to monitor key health indicators, like blood pressure or glucose, without needing the patient to step into the clinic. Patients use cellular devices at home, like blood pressure cuffs or glucose monitors, that sync data automatically to their care team.
Instead of keeping manual logs or calling in numbers, the information is shared passively and securely.
So, you might be wondering:
How Does Remote Patient Monitoring Work in Real Life?
Imagine a small primary care clinic with hundreds of chronic patients. Instead of crowding the waiting room weekly, patients now use cellular-connected blood pressure monitors, glucose trackers, and pulse oximeters at home.
Their data flows in real-time to a clinical dashboard. When something is off, say a patient’s BP spikes, the care team gets an alert. Instead of waiting for a health crisis, they intervene early via a phone call, a medicine adjustment, or a clinic visit.
Thus, RPM gives patients the dignity of daily care without daily effort, and gives clinics the ability to act faster, smarter, and more efficiently.
What are the Key Benefits of RPM for both Patients and Providers?
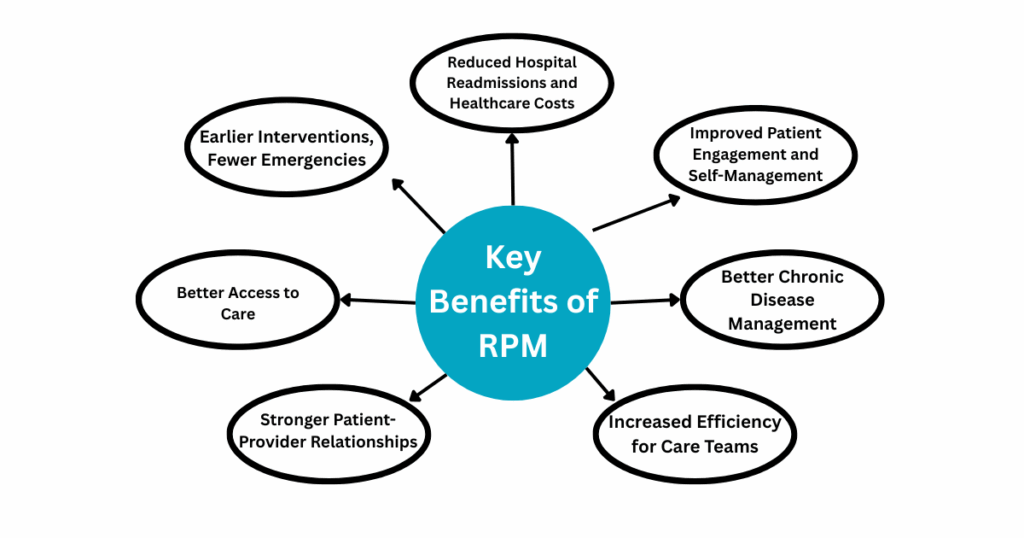
For patients, care shouldn’t stop the moment they leave the clinic. And for providers, better outcomes shouldn’t mean burnout. Remote Patient Monitoring (RPM) creates space for both, by keeping patients supported and care teams informed without overwhelming either side.
Let’s break the benefits that RPM offers to both patients and healthcare providers:
Better Access to Care
Whether it’s Carolyn living 40 minutes from her clinic or someone juggling work, kids, and chronic conditions, showing up for frequent appointments isn’t always possible. RPM bridges this gap.
With cellular-connected devices, patients can send blood pressure readings, glucose levels, and oxygen saturation from the comfort of their homes. No Wi-Fi? No problem, many devices like those offered by CandiHealth work straight out of the box with cellular connectivity.
This gives patients consistent access to monitoring and gives clinics the power to care for more people without adding more chairs in the waiting room.
Improved Patient Engagement and Self-Management
When patients track their health daily, they start spotting patterns like, “My sugar spikes when I skip breakfast.” Seeing that data in real time builds confidence and accountability.
Moreover, RPM tools often come with reminders and education prompts. making it easier for patients to stay on track. Over time, care stops feeling like an appointment, it becomes part of daily life. That quiet consistency is what leads to real, lasting change.
Earlier Interventions, Fewer Emergencies
One of the biggest advantages of RPM is catching problems before they become emergencies. When a provider sees a rising BP trend over three days, they can adjust medication or schedule a quick telehealth call. That early action can prevent a hospital admission, an ER visit, or worse.
Reduced Hospital Readmissions and Healthcare Costs
RPM has been shown to lower the chances of a patient being readmitted after discharge. When someone is monitored closely at home, especially after surgery or following a hospitalization, issues are flagged earlier, and recovery stays on track.
This directly translates to reduced healthcare costs, better resource allocation, and improved quality metrics for clinics.
Better Chronic Disease Management
Chronic illnesses like hypertension, diabetes, COPD, and heart failure need constant attention. RPM makes that possible without constant appointments.
With RPM, providers get a clearer picture of daily readings and trends. That ongoing view helps them adjust medications more accurately, offer better advice, and support patients before small issues become bigger problems.
Stronger Patient-Provider Relationships
When patients know their provider is monitoring them in real time, it builds trust. They feel seen, even when they’re not in the room. It also creates more meaningful interactions based on need, not just appointment slots.
For providers, this fosters deeper relationships without added strain. The right data at the right time leads to smarter, more personalized care.
Increased Efficiency for Care Teams
Nurses, physicians, and clinic staff manage a demanding workload; monitoring patients, reviewing reports, and responding to concerns. RPM helps make that work more manageable by offering timely insights into patient health.
With consistent updates coming in, care teams can stay organized, identify where attention is needed, and respond efficiently. It’s a more focused, less stressful way to support patients without compromising on care.
Is RPM Covered by Insurance or Medicare?
For many clinics, one of the first questions that comes up with new technology is:
“Will we get paid for using it?”
With Remote Patient Monitoring (RPM), the answer is yes.
Remote Patient Monitoring (RPM) is not only supported by Medicare, but it’s also an established pathway for generating recurring revenue while delivering better patient care.
So how does the billing side of RPM actually work? Let’s break it down
The Basics of RPM Billing
Medicare and many private insurers reimburse for RPM services using a series of CPT (Current Procedural Terminology) codes. These codes reflect different stages of RPM delivery, from device setup to ongoing monitoring.
Here’s a breakdown of the most commonly used RPM CPT codes:
CPT Code 99453
This code covers the initial setup of RPM equipment and patient education on its use. It’s billed once per episode of care.
CPT Code 99454
This code is for the supply of devices and the collection, transmission, and storage of daily patient data. It requires at least 16 days of data collection in a 30-day period.
CPT Code 99457
This code accounts for the first 20 minutes of clinical staff time spent on RPM treatment management services, including interactive communication with the patient or caregiver.
CPT Code 99458
This is an add-on code for each additional 20 minutes of RPM treatment management services beyond the initial 20 minutes covered by CPT 99457.
Source: American College of Physicians – RPM Billing & Coding Guide
RPM Billing Codes Overview
| CPT Code | What It Covers | Billing Details |
| 99453 | Initial setup of the RPM device and patient education | Billed once per episode of care |
| 99454 | Device supply, data transmission, and daily monitoring | Requires 16+ days of data in a 30-day period; billed monthly |
| 99457 | First 20 minutes of clinical staff time (review + patient contact) | Includes reviewing data and communicating with the patient monthly |
| 99458 | Each additional 20 minutes beyond the initial 99457 | Can be billed multiple times if time exceeds 20 minutes |
These codes are billable monthly, creating a steady reimbursement stream while supporting proactive care.
Unsure how these codes apply to your clinic? Contact us and we’ll walk you through it, step by step.
What Makes RPM Reimbursable?
To be eligible for reimbursement:
- The patient must have a chronic or acute condition that requires regular monitoring.
- The device used must automatically upload patient data (manual logging or phone calls don’t count).
- Data must be collected for at least 16 days within a 30-day period to qualify for billing under 99454.
- Care teams must spend and document at least 20 minutes of clinical time per month (for 99457).
How Clinics Benefit from RPM
For providers, RPM isn’t just an added service, it’s a revenue-generating tool that aligns with the shift toward value-based care. Instead of relying solely on in-person visits, RPM allows for continuous patient engagement with billing opportunities tied to meaningful interactions and outcomes.
Clinics using solutions like CandiHealth can streamline this entire process—devices are ready-to-use, data flows automatically, and time tracking for clinical engagement is built in. That means providers can focus on care, not paperwork.
Why Is RPM the Future of Healthcare?
The World Health Organization has projected a global shortage of 11 million healthcare workers in the coming years.
As chronic diseases rise and life expectancy increases, this gap will place unprecedented pressure on clinics, particularly in primary care and chronic disease management.
The future of healthcare will be defined by how well we deliver ongoing care with limited resources.
Remote Patient Monitoring (RPM) is already helping address this growing strain. By enabling providers to monitor vital signs like blood pressure, glucose levels, and oxygen saturation remotely, RPM extends care beyond the clinic without adding workload.
And the scale of adoption reflects its value.
In the United States alone, over 60 million patients are expected to use RPM tools in 2024, according to US Remote Patient Monitoring Forecast 2021. It’s a signal that RPM is delivering real outcomes: fewer hospital visits, earlier interventions, and better continuity of care.
As healthcare continues to shift toward prevention, personalization, and access, RPM checks all the right boxes.
Ready to Rethink How You Deliver Care?
Carolyn’s story isn’t unique, and neither is the strain on clinics trying to serve patients like her. The future of healthcare demands more than appointments and follow-ups. It requires care that continues, even when the visit ends.
Remote Patient Monitoring (RPM) offers a way forward. It supports patients at home, strengthens clinical decisions with real-time data, and helps healthcare teams work more efficiently.
For clinics navigating increasing patient needs, limited staff, and the shift toward value-based care, the question is no longer if RPM fits in, but how soon it should be part of the plan. Solutions like CandiHealth make that transition easier, with ready-to-use devices, automated data syncing, and built-in support for reimbursement.
Want to see how RPM can work in your clinic? Contact us—we’ll walk you through it, step by step.
Related Articles
Benefits of Remote Patient Monitoring for Patients and Providers
Remote Patient Monitoring CPT Codes: Billing & Compliance Guide
Telehealth vs. Remote Patient Monitoring: What’s the Difference?
A Comprehensive Guide to Remote Patient Monitoring Devices
Frequently Asked Questions (FAQs)
1. What is the meaning of Remote Patient Monitoring?
Remote Patient Monitoring (RPM) refers to the use of digital technologies to collect patients’ health data outside of traditional clinical settings. This data, such as blood pressure, glucose levels,, or oxygen saturation is transmitted to providers for continuous monitoring, early intervention, and better chronic disease management.
2. What is an example of remote monitoring?
A common example of remote monitoring is a patient with hypertension using a connected blood pressure monitor at home. The device automatically sends daily readings to their provider, who can then review the data, identify trends, and make adjustments to the care plan without requiring an in-person visit.
3. What does RPM mean medically?
In medical terms, RPM stands for Remote Patient Monitoring. It is a form of care delivery that allows clinicians to monitor a patient’s physiological data in real time using connected devices. RPM is especially valuable for managing chronic conditions, supporting recovery after hospitalization, and reducing unnecessary clinic visits.
4. What is the difference between Telehealth and Remote Patient Monitoring?
Telehealth involves real-time virtual visits between patients and providers, typically through video or phone. Remote Patient Monitoring (RPM), a subset of telehealth, continuously collects and transmits health data from connected devices, allowing providers to monitor patients between visits and respond proactively.