Healthcare is changing fast. Clinics are moving away from short, reactive visits toward long-term, preventive care that helps patients stay healthier and reduces costs. This shift is at the heart of Advanced Primary Care Management (APCM) — a model that builds stronger connections between providers and patients while using data to guide better decisions.
Under APCM, care teams focus on early detection, continuous monitoring, and proactive follow-up — all supported by technology like Remote Patient Monitoring (RPM) and Chronic Care Management (CCM).
According to the Centers for Medicare & Medicaid Services (CMS), value-based care programs now influence over 60% of healthcare payments in the U.S., showing how fast this model is growing.
In this blog, we’ll explore what APCM means, how it works, and why it’s becoming a key part of modern healthcare.
What is Advanced Primary Care Management (APCM)?
Advanced Primary Care Management (APCM) is a proactive healthcare model that focuses on prevention, early intervention, and care coordination instead of treating illnesses after they occur. The model relies on four main pillars:
- Proactive prevention
- Patient engagement
- Data-driven insights
- Team collaboration
These pillars work together to ensure every patient receives personalized attention rather than one-size-fits-all treatment. For example, instead of waiting for a patient’s blood pressure to reach a dangerous level, clinics using APCM monitor readings daily through Remote Patient Monitoring (RPM) systems and step in before complications arise.
Core Principles of Advanced Primary Care Management (APCM)
Advanced Primary Care Management is built on a few key principles that work together to deliver proactive, connected, and outcome-driven care. These principles guide how clinics operate under this model.
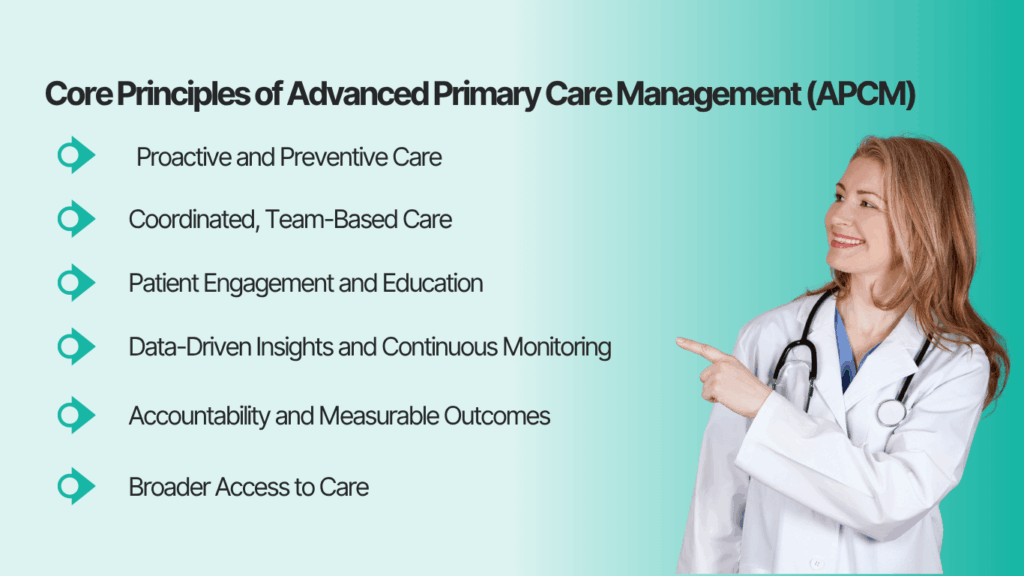
1. Proactive and Preventive Care
Instead of waiting for patients to fall sick, APCM encourages providers to stay one step ahead. Regular check-ins, wellness screenings, and health data tracking allow clinicians to identify potential risks early. For example, a patient’s rising blood pressure can trigger timely lifestyle counseling or medication adjustments before it escalates into a crisis.
2. Coordinated, Team-Based Care
APCM depends on collaboration among physicians, nurses, specialists, and care managers. Everyone involved shares a single goal, improving patient outcomes. This coordination ensures no patient “falls through the cracks,” especially those managing multiple chronic conditions. Team-based communication also reduces duplicate tests and helps providers make consistent, informed decisions.
3. Patient Engagement and Education
Patients play an active role in APCM. They’re encouraged to understand their health conditions, follow care plans, and track their progress. Educational outreach, digital reminders, and simple monitoring tools empower patients to manage their health outside clinic walls.
4. Data-Driven Insights and Continuous Monitoring
Technology forms the backbone of APCM. Tools like Remote Patient Monitoring (RPM), Electronic Health Records (EHRs), and analytics dashboards help providers collect, interpret, and act on real-time data. These insights enable early intervention and measurable outcomes — the key to thriving under value-based care models.
5. Accountability and Measurable Outcomes
Under APCM, success is measured by results, not the number of visits. Clinics track quality metrics such as hospital readmissions, medication adherence, and patient satisfaction. This accountability ensures that healthcare providers are rewarded for keeping patients healthy — aligning perfectly with CMS’s value-based reimbursement programs.
How Advanced Primary Care Management (APCM) Works in Practice
Unlike traditional care, APCM follows a structured, continuous process that keeps patients connected to their care team, both in and outside the clinic. Here’s how the workflow typically looks:
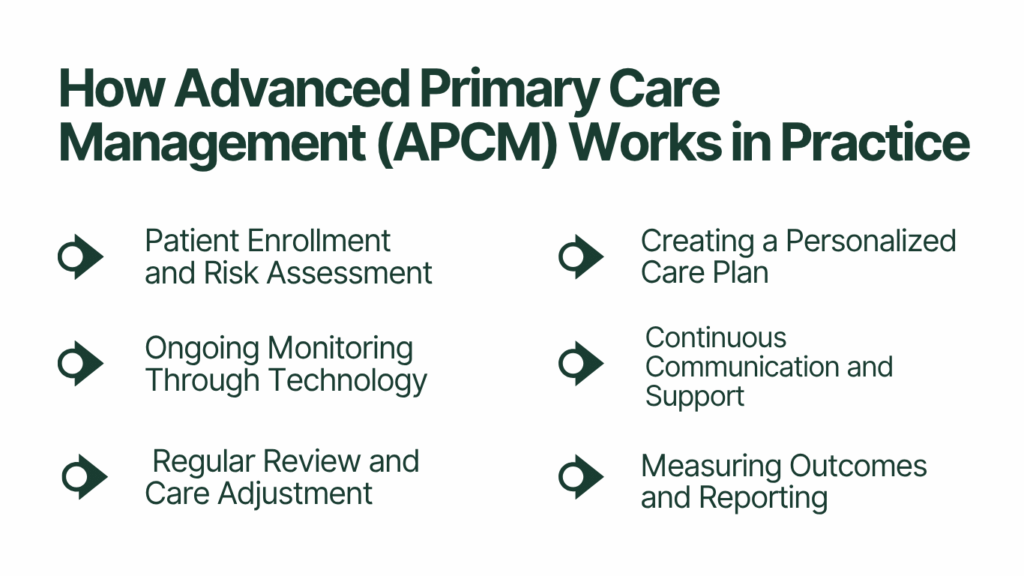
1. Patient Enrollment and Risk Assessment
The process starts with identifying eligible patients, often those with chronic conditions like hypertension, diabetes, or heart disease. After enrollment, the care team conducts a detailed baseline assessment that includes health history, vitals, and lifestyle factors. This helps determine each patient’s risk level and personalized care goals.
2. Creating a Personalized Care Plan
Each patient receives a care plan designed around their specific needs. This plan outlines medications, diet, physical activity, and scheduled monitoring. The focus is on prevention — helping patients make daily choices that reduce long-term complications.
3. Ongoing Monitoring Through Technology
This is where Remote Patient Monitoring (RPM) plays a critical role. Patients use connected devices such as cellular blood pressure monitors, glucose meters, or weight scales. These devices automatically send data to the clinic’s dashboard, allowing providers to track progress without requiring frequent visits.
4. Continuous Communication and Support
APCM emphasizes frequent communication between patients and care teams. Nurses or care coordinators check in by phone, text, or through patient portals to review readings, answer questions, or provide encouragement. These touchpoints help patients stay engaged and accountable.
5. Regular Review and Care Adjustment
At regular intervals (usually monthly), providers review data trends and health outcomes. The care plan is updated if needed — medication changes, lifestyle guidance, or specialist referrals. This cycle repeats, ensuring care remains adaptive and patient-centered.
6. Measuring Outcomes and Reporting
Finally, clinics track results using measurable indicators like blood pressure control rates, readmission reduction, and patient satisfaction scores. These metrics not only improve care quality but also influence reimbursement under value-based care programs such as Medicare’s Primary Care First or ACO REACH.
| Step | Action | Technology Used | Outcome |
| 1 | Patient enrollment | EHR, intake forms | Risk assessment completed |
| 2 | Care plan setup | Care management software | Personalized goals created |
| 3 | Ongoing monitoring | Cellular RPM devices | Real-time vitals tracking |
| 4 | Communication | Patient portal, calls | Improved adherence |
| 5 | Review & adjustment | Analytics dashboard | Optimized care plans |
| 6 | Reporting | CMS submission tools | Quality-based incentives |
The Role of Technology in Advanced Primary Care Management (APCM)
Technology is the backbone of Advanced Primary Care Management. It enables providers to move from manual, paper-based workflows to real-time, connected care systems. Let’s break down how digital tools support APCM at every level.
1. Remote Patient Monitoring (RPM)
RPM is one of the most critical technologies driving APCM forward. It allows clinics to collect patient data from home through connected devices, such as cellular blood pressure monitors, weight scales, or glucose meters.
- Patients record daily readings.
- Data is transmitted automatically to the provider dashboard.
- Care teams identify abnormal trends and intervene early.
This level of visibility turns reactive care into real-time management. For example, if a patient’s readings fall outside safe ranges, a nurse can call, adjust medication, or schedule a same-day teleconsultation.
With CandiHealth’s cellular RPM devices, clinics don’t need apps or Wi-Fi — patients simply use the device, and data is securely sent to their provider dashboard.
2. Electronic Health Records (EHR) Integration
EHRs are essential for connecting all patient data under one system. When combined with APCM, they:
- Simplify care coordination between primary and specialty providers.
- Ensure all notes, vitals, and treatment plans are updated in real time.
- Reduce errors caused by fragmented documentation.
Integrating RPM data into EHR systems further enhances clinical accuracy and ensures compliance with Medicare documentation standards.
3. Care Management Platforms
Modern APCM programs rely on platforms that unify all care tasks — scheduling, outreach, documentation, and reporting — into one place. These tools help care coordinators:
- Track patient adherence.
- Schedule check-ins automatically.
- Generate progress reports for each month.
- Submit reimbursement claims under RPM and CCM codes.
4. Predictive Analytics and AI Support
Artificial intelligence (AI) and predictive analytics are now being used to identify at-risk patients even before symptoms worsen. By analyzing data trends, AI tools can:
- Predict potential hospitalizations.
- Suggest care plan adjustments.
- Highlight patients with low engagement levels.
5. Telehealth and Communication Tools
Telehealth extends the reach of APCM beyond clinic walls. Patients can have virtual consultations, receive medication counseling, or review their monitoring results remotely. Combined with secure messaging and automated reminders, it keeps engagement strong and reduces missed appointments.
Final Thoughts
Advanced Primary Care Management (APCM) is the blueprint for the future of healthcare. By focusing on prevention, data-driven insights, and ongoing engagement, APCM transforms the way clinics care for patients. It closes the gap between in-person visits and daily health management, ensuring that patients stay supported every step of the way.
The most effective APCM programs combine human connection with smart technology, and that’s where tools like CandiHealth make the difference. CandiHealth’s Medicare-compliant platform simplifies Remote Patient Monitoring (RPM) with preconfigured cellular devices, automated dashboards, and flat-rate pricing. It gives clinics everything they need to deliver high-quality, continuous care.