A 2024 JAMA Health Forum study found that nearly 1 in 5 RPM programs experience device-related interruptions within the first six months of implementation. Sometimes it’s a simple battery issue; other times, a deeper software or connectivity fault that silently disrupts data flow.
And because most patients rely on these devices without constant supervision, such failures can go unnoticed for days, creating blind spots in care.
For patients, this means missed alerts or delayed treatment. For clinics, it means data gaps, frustrated staff, compliance issues, and lost trust. Yet, these technical breakdowns are rarely discussed in detail. Many RPM vendors highlight the convenience, but few talk about the practical realities when a device fails.
In this blog, we’ll unpack what really happens when an RPM device stops working, the hidden pitfalls, and how both patients and clinics can prepare for these challenges.
What Happens When the RPM Device Stops Working?
When an RPM device stops working, data transmission halts — meaning your doctor no longer receives your daily readings. Depending on the issue, it might record inaccurate values, stop syncing entirely, or display an error. For patients, this can cause false reassurance or panic. For clinics, it leads to gaps in monitoring, missing alerts, and compliance risks under Medicare billing requirements.
In simple terms, when the device fails:
- The data flow breaks, leaving doctors blind to a patient’s condition.
- Alerts stop triggering, so critical changes may go unnoticed.
- Reports become unreliable, which affects documentation and reimbursements.
- Patient confidence drops, often leading to disengagement from the RPM program.
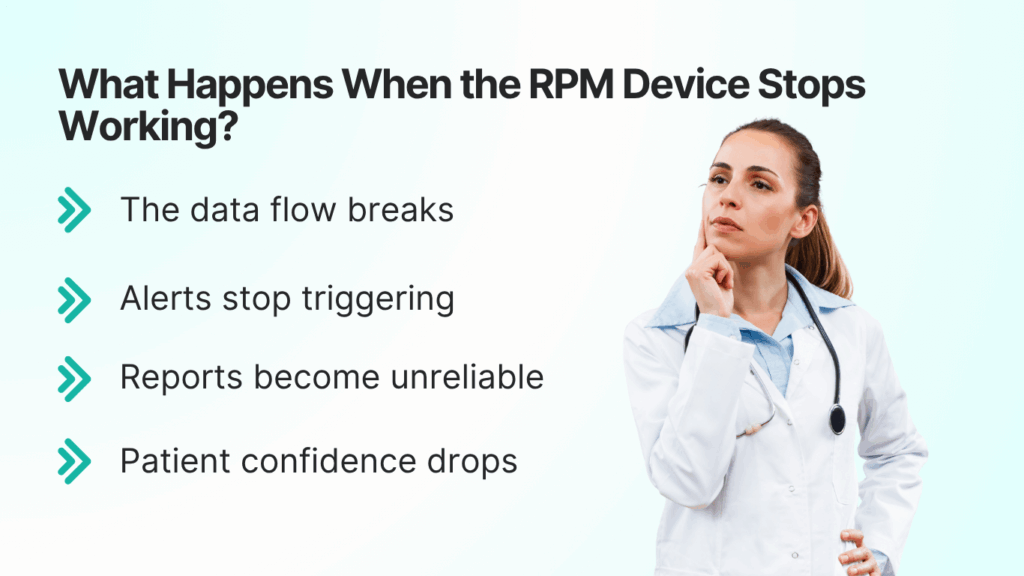
While these failures are uncommon in reliable systems, they highlight why technical reliability matters as much as medical accuracy.
How and Why RPM Devices Fail (Technical Failure Modes)
Even the best remote patient monitoring device can fail — not because it’s poorly made, but because it relies on multiple small parts working in harmony. When one link in that chain breaks, the whole system stops sending accurate data.
Common Causes of RPM Device Failure
| Failure Type | What Happens | Example |
| Battery or Power Issue | Device shuts off or gives false readings when charge is low. | BP monitor turns off mid-reading. |
| Connectivity Drop | Bluetooth or cellular signal disconnects from the hub or app. | Rural patients often face this. |
| Sensor Malfunction | Internal sensors wear out or get dirty, sending incorrect data. | Temperature sensors show 98.6 °F all the time. |
| Software Bug | App crashes or stops syncing data to the portal. | Update causes loss of previous readings. |
| Firmware Corruption | Device fails to boot or continuously reboots. | After firmware update, device won’t connect. |
| Human Error | Patients misuse or forget calibration steps. | Incorrect cuff placement for BP monitors. |
According to a 2024 IEEE Sensors Journal review, over 30 % of device failures in RPM programs are related to connectivity or battery issues, followed by 18 % due to human error.
Early Warning Signs of a Failing Device
- Unusual or repetitive readings (e.g., identical numbers daily)
- Long sync delays between readings and the portal
- Device heating, freezing, or flashing abnormal indicators
- Missing data alerts from the clinician dashboard
Recognizing these signs early helps clinics act before it affects care quality.
Impact on the Patient: Safety, Data Gaps & Trust
When an RPM device stops working, the first and most critical impact is on patient safety. These devices are designed to detect subtle health changes before they escalate, but when data stops flowing, those early warnings disappear.
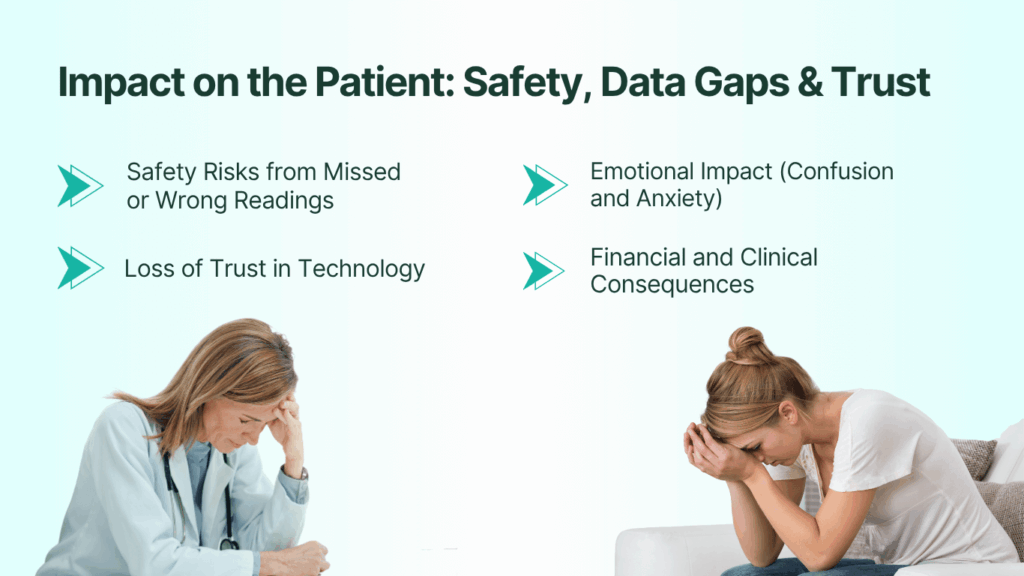
1. Safety Risks from Missed or Wrong Readings
A broken or disconnected device can create two kinds of danger:
- Missed alerts: The system can’t warn a doctor if blood pressure spikes or oxygen drops.
- False reassurance: If readings freeze or display incorrect values, patients may think everything is fine when it’s not.
A 2023 American Heart Association report noted that 8–10% of patients in RPM programs for hypertension experienced missed alerts due to device errors or connectivity issues. Even short gaps, as little as 24 hours, can affect timely clinical response.
2. Emotional Impact: Confusion and Anxiety
When patients notice their readings aren’t updating or the app shows errors, anxiety rises. Some lose confidence in the entire system. This often leads to:
- Frustration or withdrawal from the program.
- Reduced adherence to daily monitoring.
- Delayed communication with their provider.
In long-term care programs, this emotional disconnection can quietly undo months of progress in patient engagement.
3. Loss of Trust in Technology
Trust is the foundation of RPM success. Once patients experience repeated technical failures, they start doubting not only the device but also the clinic’s reliability. This “trust fatigue” spreads through word-of-mouth — and can lower enrollment rates in RPM programs.
4. Financial and Clinical Consequences
If patients disengage or skip readings:
- Medicare compliance drops (RPM requires 16 days of data per month for billing).
- Clinical outcomes worsen due to gaps in trend data.
- Follow-up visits increase, costing both patients and providers more time.
Impact on the Clinic: Workflow, Liability & Data Integrity
When an RPM device fails, the clinic feels the ripple effects almost immediately. What seems like a small technical glitch on the patient’s end can create major workflow disruption, compliance challenges, and data reliability issues inside the clinic.
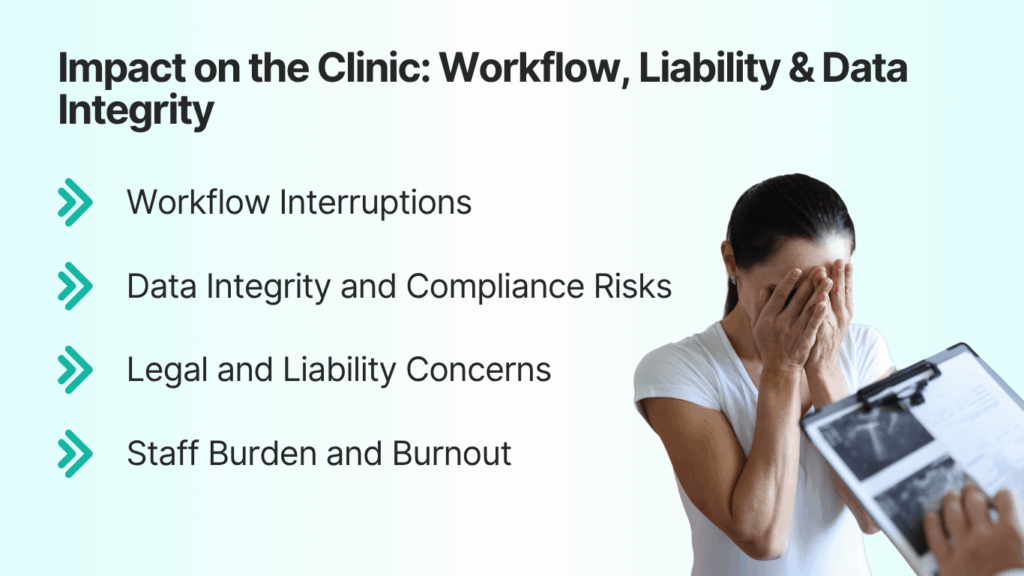
1. Workflow Interruptions
Clinicians depend on daily readings to make care decisions. If those readings stop coming in:
- Staff must manually follow up with patients to check what went wrong.
- The nurse or care coordinator spends time troubleshooting devices instead of focusing on care.
- Scheduled reviews and reports are delayed, creating administrative backlogs.
Over time, these interruptions drain efficiency and morale. Clinics running large RPM programs may spend up to 10 extra staff hours per week resolving device issues, according to a 2024 Healthcare IT News survey.
2. Data Integrity and Compliance Risks
Data is the backbone of every RPM claim. A missing or corrupted data stream can lead to:
- Incomplete patient records, which reduce accuracy in clinical decision-making.
- Non-compliance with CMS billing rules, as continuous monitoring data is required for CPT codes 99454–99458.
- Audit exposure, since missing data points can raise red flags during claim reviews.
Even one malfunctioning device across multiple patients can skew clinical reports and reimbursement metrics.
3. Legal and Liability Concerns
When a device fails and a health incident follows, clinics may face tough questions:
- Did the clinic act fast enough?
- Was the device maintained properly?
- Who is responsible — the provider or the vendor?
Under current RPM liability frameworks, clinics are expected to show reasonable oversight of device function. A pattern of missed readings without documented follow-up can pose legal and ethical challenges.
4. Staff Burden and Burnout
Device-related problems can quietly increase staff burnout. Instead of focusing on proactive care, nurses often handle repetitive tech issues — Bluetooth pairing, reconnections, or patient complaints. Over time, these micro-delays can reduce satisfaction and contribute to staff turnover.
Prevention & Response: What Patients & Clinics Should Do
When a remote-monitoring device stops working, speed and clarity matter more than panic. Both patients and clinics can prevent most problems or at least limit their impact, by following a few practical steps.
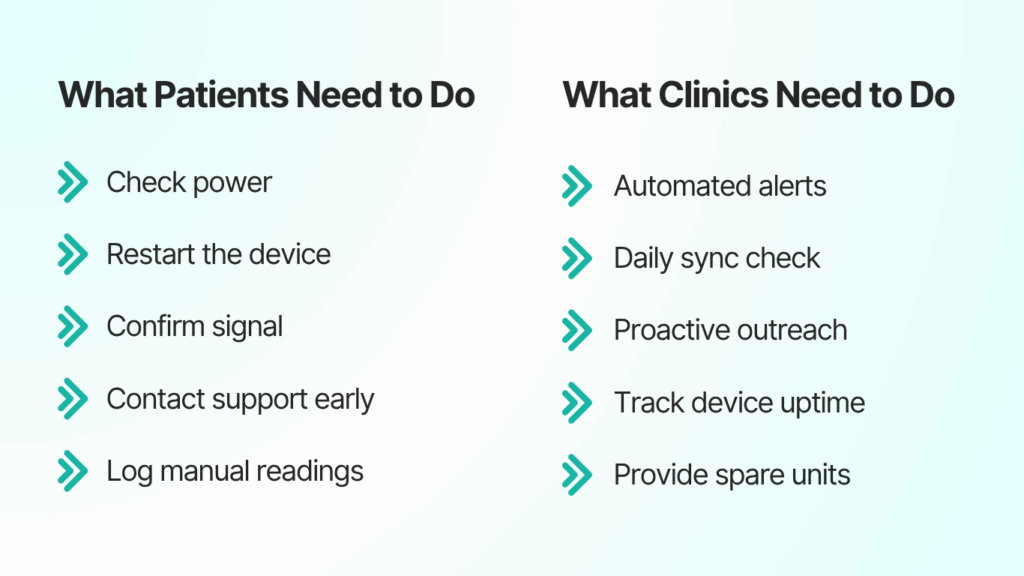
1. What Patients Need to Do
If your readings suddenly look identical for days or your device flashes unusual lights, it’s time to act.
What to do immediately:
- Check power: Make sure batteries or charging cables are properly connected.
- Restart the device: A quick reboot resolves many Bluetooth or cellular issues.
- Confirm signal: Ensure you’re in an area with stable cellular or Wi-Fi coverage.
- Contact support early: Don’t wait for your next appointment; notify the clinic or vendor as soon as you suspect an error.
- Log manual readings if possible until the issue is fixed.
2. What Clinics Need to Do
Every RPM program should include a step-by-step response when device data stops flowing.
Best practices for clinics:
- Automated alerts: Use dashboards that flag missing data within 24 hours.
- Daily sync check: Assign one staff member to review incoming transmissions.
- Proactive outreach: Call patients after two missed days, not two weeks.
- Track device uptime: Keep a monthly reliability log for audits and billing documentation.
- Provide spare units: Maintain a small buffer stock to avoid downtime.
Staff tip: Train nurses and care coordinators to recognize early technical red flags — like delayed syncs or repetitive data patterns — so intervention happens before a compliance gap forms.
Conclusion: Reliability Isn’t Optional in Remote Care
When an RPM device stops working, it’s a break in the trust and continuity that remote care depends on. The fallout affects everyone: patients lose confidence, clinics lose data integrity, and outcomes become harder to measure.
The truth is, even the smallest glitch — a weak signal, a drained battery, or a software lag — can interrupt the flow of life-saving information. That’s why proactive prevention, transparent communication, and vendor accountability are essential.
Reliable remote monitoring isn’t about avoiding every failure; it’s about detecting, managing, and preventing small problems before they become serious.
How CandiHealth Prevents Downtime Before It Starts
At CandiHealth, device reliability isn’t an afterthought — it’s a core promise.
- Automatic device health checks detect anomalies early.
- Cellular connectivity ensures readings transmit without apps or Wi-Fi.
- 24/7 monitoring & early replacement mean no patient is left untracked.
- Encrypted backups keep every reading safe and compliant.
Whether you manage ten patients or a thousand, CandiHealth keeps your data — and your care — flowing seamlessly.
Learn more about how CandiHealth keeps your RPM program reliable and worry-free. Explore CandiHealth RPM Solutions →
Frequently Asked Questions (FAQs)
What should I do immediately if my RPM device stops working?
If your remote patient monitoring (RPM) device stops working, check the battery, restart the device, and confirm connectivity. Take manual readings if possible and contact your clinic or vendor support immediately. Quick action ensures your doctor continues to receive accurate, real-time health data without interruption.
How long can a data gap go undetected before it becomes a clinical risk?
Even short gaps (24–48 hours) in reliable data flow can hamper timely clinical intervention and disrupt trend-analysis. Regular uptime monitoring is essential to prevent small gaps from becoming serious care risks.
Who is responsible when a device fails — the patient, the vendor, or the clinic?
Responsibility is shared: the patient needs to use the device properly (charging, location, instructions); the vendor must provide reliable hardware/firmware and support; the clinic must monitor data flow and respond when issues arise. Clear protocols help prevent blame-shifting.
Can a device that appears to be working still be providing inaccurate data?
Yes. For example, calibration drift (sensors gradually losing accuracy), stale cached data, or connectivity issues that delay sync can lead to false readings or false “normal” values. These hidden failures are among the technical pitfalls seldom discussed.