Remote Patient Monitoring (RPM), also called remote physiologic monitoring, is one of the fastest-growing areas of healthcare in the United States. It allows providers to track patients’ health data outside the hospital setting, using connected medical devices that transmit information securely.
Over the last few years, RPM has been widely embraced by physicians, patients, Medicare, and commercial insurers. Understanding remote patient monitoring examples helps make the concept more practical. Because these real-world examples show how RPM directly benefits patients and providers.
Continue reading this blog to learn how it is transforming chronic disease management, post-hospital care, and long-term health monitoring across specialties like cardiology, pulmonology, and endocrinology.
Table of Contents
Remote Patient Monitoring Examples for Cardiovascular Conditions
Cardiovascular disease remains the leading cause of death in the United States, with conditions such as hypertension, heart failure, and obesity requiring continuous oversight. These conditions are particularly well-handled with remote patient monitoring (RPM) because they involve vital signs that can change quickly and often without obvious symptoms.
By using connected medical devices, cardiologists gain access to timely data that supports early intervention, reduces complications, and helps prevent costly hospitalizations.
1. Hypertension Management with RPM Devices
Nearly 47.7% of U.S. adults have hypertension, yet control rates remain low — only about one in four manage to keep their blood pressure within target ranges (CDC). Because hypertension often does not show obvious symptoms, regular home monitoring is essential.
With RPM blood pressure cuffs, patients can track their readings at home, and the data is transmitted automatically to their providers. This allows clinicians to make timely adjustments to medications and lifestyle recommendations. Remote blood pressure monitoring has been shown to improve control rates and reduce risks of stroke and heart disease.
With platforms like CandiHealth, providers can automate the collection of blood pressure data, receive real-time alerts, and streamline follow-up care. This ensures that hypertension management is proactive, efficient, and less burdensome for both patients and clinicians.
2. Medication Adjustment and Management
Effective hypertension treatment often requires ongoing adjustments to medications. Research shows that about 77.4% of U.S. adults with hypertension remain uncontrolled despite treatment, due in part to suboptimal medication management (JAMA Network).
By receiving continuous blood pressure data through RPM, physicians can adjust medications more safely and effectively. This reduces the trial-and-error gap in treatment and ensures patients get the right combination of therapies sooner.
3. Weight Monitoring for Congestive Heart Failure (CHF)
One of the earliest warning signs of worsening heart failure is sudden weight gain due to fluid retention. With connected weight scales, RPM programs enable patients to record daily weights, which are then shared with their care team.
This allows providers to detect fluid buildup early and intervene with medication adjustments before the patient requires hospitalization. Studies consistently show that daily weight monitoring reduces rehospitalizations in CHF patients.
4. Weight Monitoring for Obesity
Obesity affects more than 40% of American adults, making it one of the most significant risk factors for cardiovascular disease (CDC). With RPM, patients can track their weight trends over time, and providers can use this information to guide behavior change programs, diet plans, and medication-assisted weight management.
Unlike traditional care, which relies on sporadic office visits, connected scales provide continuous feedback that helps patients stay accountable and allows providers to tailor interventions in real time.
Remote Patient Monitoring Examples for Respiratory Conditions
Remote patient monitoring (RPM) provides pulmonologists with continuous insights into patients’ respiratory health, supporting proactive care and reducing risks.
1. COPD Monitoring with Pulse Oximeters
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death by disease in the United States, affecting about 12.5 million Americans with a formal diagnosis, while millions more remain undiagnosed (American Lung Association). Patients with COPD often experience sudden drops in oxygen saturation that can lead to severe exacerbations.
With RPM, patients can use connected pulse oximeters to measure oxygen levels at home, transmitting data directly to their providers. This allows clinicians to make timely adjustments to treatment, such as oxygen therapy or medication changes, helping to reduce emergency visits and hospitalizations.
2. Asthma Monitoring with Respiratory Devices
Asthma affects more than 27 million Americans, including 4.5 million children, making it one of the most common chronic respiratory conditions (CDC). Management often requires monitoring lung function and ensuring proper use of inhalers.
Through RPM, patients can use electronic peak-flow meters, connected inhaler sensors, or home spirometers. These tools give providers daily insights into lung function, symptom control, and medication adherence. Studies have shown that continuous monitoring helps improve symptom-free days and reduces reliance on rescue medication.
3. Other Respiratory Diseases
RPM is also expanding into the management of cystic fibrosis, which affects about 40,000 people in the United States, and bronchiectasis, which is increasingly recognized in older adults (Cystic Fibrosis Foundation).
For these conditions, connected remote patient monitoring devices such as spirometers and pulse oximeters help providers detect subtle declines in lung function or oxygen levels earlier. This supports quicker interventions and better adherence to long-term therapies, improving patient quality of life.
Remote Patient Monitoring Examples in Endocrine & Metabolic Conditions
Endocrine and metabolic conditions like diabetes and obesity are among the most widespread chronic health problems in the United States.
1. Glucose Monitoring for Diabetes
Diabetes affects more than 38 million Americans, representing about 11.6% of the population, with 1.2 million new cases diagnosed annually (CDC). Blood glucose monitoring is essential for adjusting medications, evaluating dietary choices, and tracking progress toward treatment goals.
RPM-enabled glucose meters allow patients to test at home while automatically sharing results with their care team. Providers can then adjust insulin or oral medications more effectively. Evidence shows that remote monitoring programs for diabetes help lower HbA1c levels, improving long-term control and reducing complications.
2. Continuous Glucose Monitoring (CGM)
For people with type 1 diabetes, and some with type 2, continuous glucose monitoring is considered a best practice. A CGM uses a small sensor under the skin to record glucose levels throughout the day.
The U.S. Food and Drug Administration (FDA) reports that CGM provides more comprehensive insight into glucose fluctuations. When integrated into RPM platforms, CGM devices transmit data directly to providers, enabling real-time alerts for dangerously high or low levels.
This continuous feedback helps prevent severe episodes of hypoglycemia or hyperglycemia and guides fine-tuned adjustments to therapy.
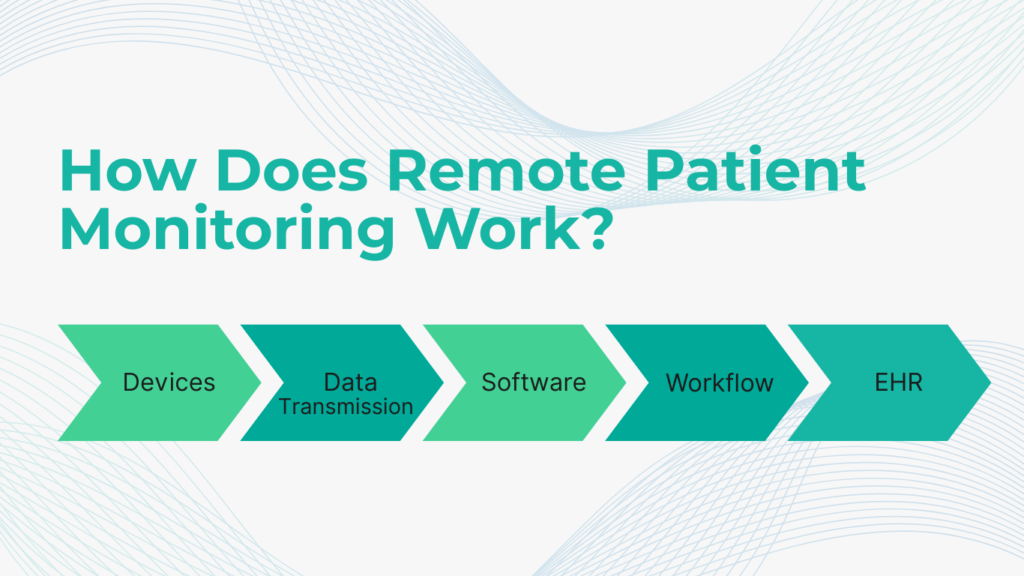
How Does Remote Patient Monitoring Work?
Remote patient monitoring (RPM) may sound complex, but the process is straightforward. It combines FDA-approved medical devices with secure technology platforms to deliver continuous insights to providers. Here’s how it works in practice:
1. Patient Measures Health Data with Connected Devices
Patients are given connected medical devices such as a blood pressure cuff, glucose meter, pulse oximeter, or weight scale. These devices are easy to use and require little to no technical setup from the patient’s side.
2. Health Data Is Collected Automatically
Each time a patient takes a reading, the device records the result. Unlike traditional home monitoring, where patients write down values in a logbook, RPM devices automatically capture the data.
3. Data Is Transmitted Securely to the RPM Platform
The collected information is transmitted securely to a cloud-based RPM platform. Depending on the device, this can happen via Bluetooth, cellular connection, or Wi-Fi.
4. Providers Review Results Through a Clinical Dashboard
Providers access a digital dashboard that organizes patient data into trends and alerts. For example, a sudden spike in blood pressure or drop in oxygen saturation would be flagged for review.
5. Providers Take Action Based on Data
Based on the incoming data, providers can adjust medications, schedule follow-up calls, or recommend lifestyle changes. Many RPM programs also include messaging tools that allow real-time communication between patients and care teams.
FAQs: Common Questions on Remote Patient Monitoring Examples
What is an example of patient monitoring?
A simple example of patient monitoring is daily weight measurement in heart failure patients. Tracking these changes helps identify fluid retention early, which is often a warning sign of worsening heart failure.
What is an example of remote patient monitoring (RPM)?
Continuous glucose monitoring (CGM) for diabetes is a strong example of RPM. A CGM sensor tracks glucose levels around the clock and transmits data to a provider dashboard, supporting timely medication and insulin adjustments.
What are remote patient monitoring systems?
Remote patient monitoring systems combine devices, software platforms, and care team workflows to deliver continuous patient data to providers. These systems may include blood pressure monitors, glucose meters, or pulse oximeters, all connected to a secure dashboard that providers use for decision-making.
Final Thoughts
Remote patient monitoring is becoming a core part of modern healthcare. These examples of remote patient monitoring show how simple devices and smart systems can transform care outside the walls of hospitals and clinics.
RPM gives better access to timely data, proactive decision-making and stronger patient engagement to healthcare providers. It represents a shift toward preventive, value-based care that improves patient outcomes.
Clinics that adopt RPM today are building stronger connections with their patients and creating a more sustainable model of care for tomorrow.
Ready to bring the benefits of remote patient monitoring to your practice? CandiHealth helps clinics launch and scale RPM programs with preconfigured devices, seamless provider dashboards, and full compliance support. Book a free demo today to see how we can help your team deliver smarter care.