Table of Contents
Remote Patient Monitoring has helped clinics improve care and reduce readmissions. One study found that patients with hypertension saw a 7 mm Hg drop in blood pressure after 90 days of using RPM. Moreover, The University of Pittsburgh Medical Center reported a 76 % reduction in readmissions and over 90 % patient satisfaction after RPM adoption
These results show the real impact of RPM. But starting with it isn’t always easy.
Many clinics face challenges including setup problems, poor patient compliance, and unclear billing processes. If not addressed early, they can slow down adoption or cause programs to fail.
This blog outlines the most common challenges providers face with RPM, and how to solve them using practical, proven steps.
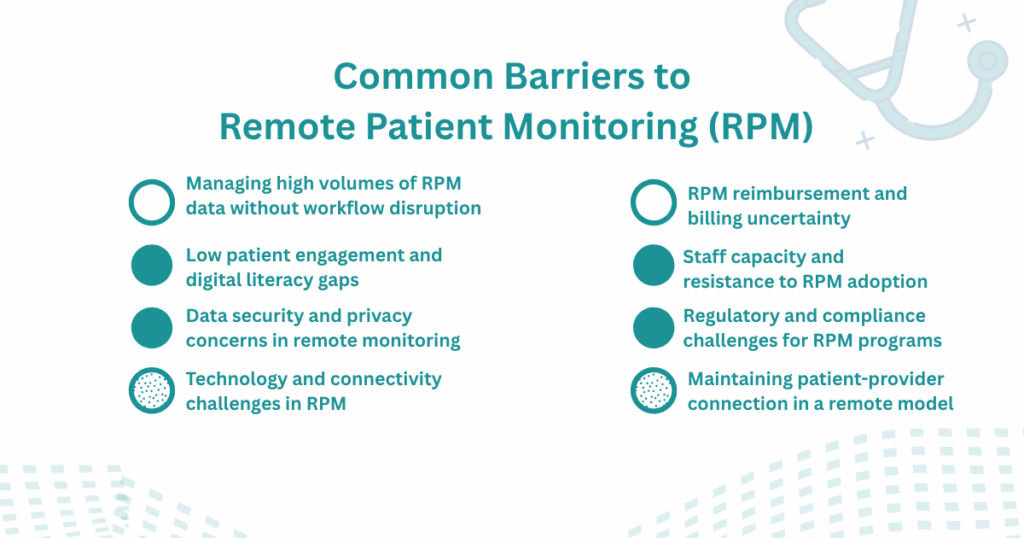
Common Barriers to Remote Patient Monitoring (RPM)
Even when clinics see the value in Remote Patient Monitoring, many struggle to make it work day to day. Based on real-world feedback from providers and studies across healthcare systems, these are the most common challenges:
- Technology and connectivity challenges in RPM
- Low patient engagement and digital literacy gaps
- Managing high volumes of RPM data without workflow disruption
- Data security and privacy concerns in remote monitoring
- RPM reimbursement and billing uncertainty
- Staff capacity and resistance to RPM adoption
- Regulatory and compliance challenges for RPM programs
- Maintaining patient-provider connection in a remote model
Here’s a breakdown of each barrier and how clinics are solving them.
1. Technology and Connectivity Challenges in RPM
One of the most common challenges to Remote Patient Monitoring implementation is the technology itself. Patients often find it difficult to connect devices or keep them running. In some cases, internet access is limited. In others, patients aren’t comfortable handling health devices on their own.
These issues often lead to missed readings, delayed interventions, and, in some cases, complete disengagement from the program. From the provider’s side, technical support becomes a recurring burden, consuming staff time and slowing down scale.
Solution: Reduce Technical Friction at the Start
One of the most effective ways to address these barriers is to remove technical responsibility from the patient side as much as possible. This means avoiding systems that require app downloads, Wi-Fi setup, or Bluetooth pairing.
Platforms like CandiHealth support this model by offering cellular-enabled devices that are configured before reaching the patient. Once the device is turned on, it begins transmitting data directly to the care team—no apps, no logins, no setup required.
This simplifies the process for patients, reduces reliance on tech literacy, and allows providers to monitor consistently from the start.
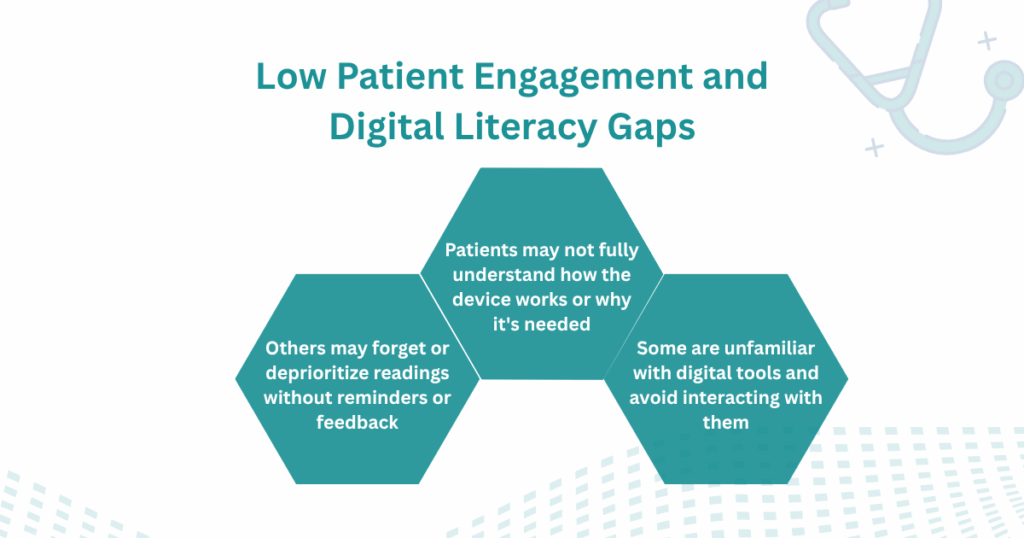
2. Low Patient Engagement and Digital Literacy Gaps
Remote Patient Monitoring depends on consistent participation, but many programs struggle to maintain it. Even when devices are delivered and active, some patients don’t take regular readings or stop using the equipment altogether.
Several factors that contribute to low patient engagement
- Patients may not fully understand how the device works or why it’s needed.
- Some are unfamiliar with digital tools and avoid interacting with them.
- Others may forget or deprioritize readings without reminders or feedback.
These issues result in incomplete data and lower program effectiveness, especially in populations with limited access to digital technology.
Recommendation: Keep Participation Simple and Clear
To address these gaps, clinics should focus on simplifying the patient experience and improving communication.
Devices that require no apps or logins tend to see better retention. Basic support materials, such as printed instructions or scheduled follow-up calls, can also improve comfort and reduce drop-off.
Supporting engagement early improves long-term results and reduces the need for manual follow-up later.
3. Managing High Volumes of RPM Data Without Workflow Disruption
As more patients enroll in RPM programs, care teams begin receiving large volumes of readings; blood pressure, glucose, heart rate, oxygen saturation, and more.
But without a system to triage and prioritize the information, staff end up reviewing every entry manually. This increases administrative workload and introduces the risk of missing clinically important trends.
How can clinics manage this more efficiently?
The key is to structure the flow of data in a way that matches clinical capacity. This includes:
- Setting thresholds to highlight only clinically relevant readings
- Using dashboards that organize patient data by priority
- Assigning dedicated staff or care coordinators to monitor incoming data
Some RPM platforms like Candihealth now offer built-in logic to filter readings, group patients by risk level, and generate only the alerts that need a response. This helps providers avoid data overload and focus on meaningful intervention.
4. Data Security and Privacy Concerns in Remote Monitoring
Remote Patient Monitoring depends on the secure transmission of personal health information between patients and providers. With this comes a responsibility to protect data at every stage, from the device to the clinic’s systems.
Below are common risks providers face, alongside strategies used to reduce them:
| Risk | Mitigation Strategy |
| Unsecured data transmissionPatient data may be intercepted if transmitted over open networks. | Use encrypted cellular connections instead of Wi-Fi or public internet. Devices should support HIPAA-compliant transmission protocols. |
| Unauthorized accessShared devices or accounts can lead to unintended access by family members or others. | Implement secure device authentication and provider-side access controls. Role-based permissions help limit exposure. |
| Data breaches at storage levelEven if data is securely transmitted, poor storage practices can result in breaches. | Partner with platforms that maintain end-to-end security and are audited against recognized standards (e.g., SOC 2, HITRUST). |
| Unclear patient consentPatients may not fully understand what is being monitored or how their data is used. | Provide written consent forms during onboarding and explain data usage in clear, accessible language. |
RPM programs that prioritize security from the outset are better positioned to maintain trust and meet compliance standards. Platforms like CandiHealth are designed with built-in encryption, secure storage practices, and support for HIPAA-aligned workflows, reducing the administrative effort needed to maintain compliance.
5. RPM Reimbursement and Billing Uncertainty
Many clinics enter the RPM program without fully understanding the billing implications. Some vendors or billing services deduct a share of reimbursement revenue. While this may be part of the service model, it’s often unclear or underestimated.
Moreover, staff may lack up-to-date knowledge of RPM-specific CPT codes such as 99453 (setup), 99454 (device supply), 99457 (monitoring with communication), and 99458 (additional time).
Medicare requires detailed documentation for each, including time tracking and monthly patient interactions. Without a structured approach to billing, clinics often miss eligible reimbursements or submit claims that do not meet payer requirements. Over time, this raises concerns about the financial sustainability of the program.
Recommended Approach: Build Billing Into the Operational Workflow
Clinics should review any vendor or billing partner agreements carefully to understand how revenue is split and what reporting is needed. Internally, teams should receive CPT code training tied to daily workflows, with tools in place to track time, document patient communications, and log consent appropriately.
Platforms like CandiHealth support this model by aligning device data with CPT billing requirements, automatically tracking time, and simplifying documentation. This helps clinics improve reimbursement accuracy without adding to administrative overhead.
6. Staff Capacity and Resistance to RPM Adoption
Even when leadership is aligned and the technical systems are in place, RPM programs often face resistance from clinical staff. Here are three key reasons RPM adoption may slow down at the staff level:
1. Competing Priorities
Nurses, medical assistants, and care coordinators already manage full patient loads, documentation requirements, and in-clinic responsibilities. RPM can be seen as one more system to manage, especially if workflows aren’t clearly defined.
2. Lack of Role Clarity
Unclear task ownership, such as who is responsible for reviewing incoming data, responding to alerts, or logging time for billing, can create confusion and lead to delays or incomplete follow-through.
3. Limited Training or Support
If RPM systems are introduced without adequate hands-on training or support, staff may default to minimal engagement. In some cases, resistance stems from uncertainty, not unwillingness.
Recommended Approach
To improve staff adoption, clinics should assign clear roles, reduce unnecessary steps, and ensure proper onboarding. With defined responsibilities and ongoing support, staff can view RPM as a care extension—not an added burden.
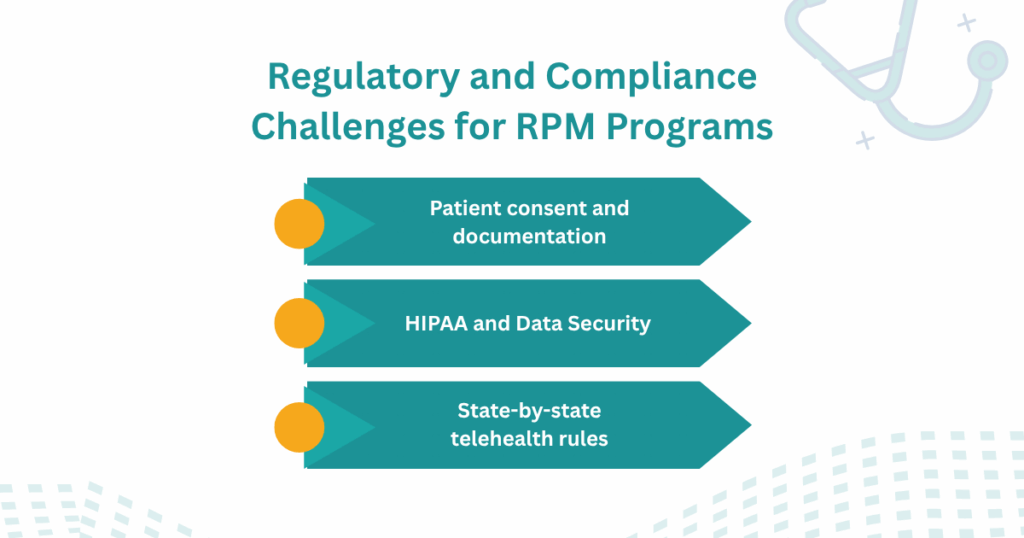
7. Regulatory and Compliance Challenges for RPM Programs
While RPM is supported by CMS and commercial payers, the legal and procedural requirements are often misunderstood or overlooked, especially during scale-up.
RPM compliance challenges typically fall into three areas:
- Patient consent and documentation: Providers must secure and record informed consent before billing, in a format that meets both Medicare and state-level requirements
- HIPAA and data security: RPM systems must comply with HIPAA standards across data transmission, storage, and access. This applies to every device, platform, and third-party vendor involved in care delivery.
- State-by-state telehealth rules: Licensing, remote prescribing rights, and documentation standards can vary by state, particularly for multi-state or network-based providers.
Failure to meet these requirements result in claim denials, audits, or reputational damage.
Recommended Approach: Align RPM Workflows with Regulatory Requirements
Regulatory compliance in RPM is an operational necessity. Clinics should establish internal protocols for consent, ensure all vendors follow HIPAA-compliant practices, and routinely audit systems for adherence to CMS billing rules.
Building compliance into daily operations allows RPM programs to scale confidently and stay audit-ready from day one.
8. Maintaining Patient–Provider Connection in a Remote Model
A nurse at a primary care clinic recently shared a concern during an RPM training session:
“One of my long-time patients used to come in every two weeks. Now we receive her readings, but I haven’t spoken to her in months.”
This reflects a common concern with remote monitoring. As in-person visits decrease, some patients begin to feel disconnected from their care team. At the same time, providers lose the opportunity to observe physical cues or have unstructured conversations that often help guide care decisions.
Keeping Communication Part of the Workflow
To maintain continuity, clinics can schedule regular check-ins, by phone or video, regardless of whether readings are within range. A brief conversation once a month may be enough to support trust and clarify any issues the data doesn’t show.
Monitoring platforms that include simple messaging tools or flags for missed readings can also help teams stay connected. These small steps create space for direct communication without requiring a full appointment.
Final Thoughts
Remote Patient Monitoring offers benefits to both patients and providers. It supports timely care, reduces unnecessary visits, and allows clinics to manage chronic conditions more effectively. But starting and sustaining an RPM program is not without challenges.
From technical issues and low patient engagement to billing complexity and regulatory pressure, the success of an RPM program depends on how these barriers are addressed. Clinics that take a structured approach—one that aligns workflows, simplifies patient use, and supports staff—are more likely to see long-term results.
Platforms like CandiHealth help clinics manage this process by combining simplified technology, built-in compliance tools, and support for billing integration. While no system removes every barrier, the right tools can make RPM more reliable, more manageable, and more effective.
Related Articles
Remote Patient Monitoring CPT Codes: Billing & Compliance Guide
Frequently Asked Questions (FAQs)
1. What are the challenges of remote patient monitoring?
Remote Patient Monitoring (RPM) offers several challenges for clinics and healthcare providers. These include technology-related issues such as device setup difficulties and unreliable connectivity, low patient engagement due to digital literacy gaps, and administrative burdens tied to billing and compliance.
2. What are the challenges in managing a remote monitoring device clinic?
Managing a remote monitoring device clinic involves coordinating device logistics, ensuring data accuracy, training staff, and supporting patients, especially those unfamiliar with health technology.
Clinics must also handle documentation, billing under CPT codes, and regulatory compliance. Without integrated systems and clear task assignments, these responsibilities can overwhelm clinical teams and impact program performance.
3. What are the disadvantages of a remote monitoring system?
While remote monitoring improves access and early intervention, disadvantages include reduced face-to-face interaction, patient dropout due to technical frustration, and the risk of data overload for providers.
If systems lack proper filters or triage tools, staff may struggle to identify which readings require attention. Additionally, privacy and reimbursement concerns remain ongoing considerations in many care settings.