Table of Contents
Telehealth vs RPM is one of the most discussed comparisons in remote patient care.
The core difference lies in how care is delivered and what kind of data is captured.
Telehealth involves real-time communication—such as video or phone calls—between a patient and a provider for consultations, follow-ups, or behavioral health check-ins.
Remote Patient Monitoring (RPM), on the other hand, uses connected medical devices (like blood pressure cuffs or glucose meters) to collect and transmit biometric data continuously—without needing a live interaction.
Both fall under the broader category of virtual care, but they serve distinct clinical purposes. Telehealth is interaction-based; RPM is data-driven and designed for ongoing monitoring, especially for patients with chronic conditions.
For a deeper understanding, including benefits, and a side-by-side comparison, read the full breakdown below.
What is Telehealth?
Telehealth refers to the remote delivery of clinical services through live, two-way communication between a patient and a provider. These sessions are usually conducted via video, but may also include phone calls or secure messaging, depending on the patient’s needs and the nature of the appointment.
Telehealth is most commonly used for:
- Virtual consultations
- Health assessment
- Routine follow-up appointments
- Medication management and supervision.
- Behavioral health sessions
Telehealth improves access to care, particularly for patients in rural or underserved areas, and offers flexibility for both patients and providers. But once the session ends, visibility into the patient’s health status stops until the next check-in.
What is Remote Patient Monitoring (RPM)?
As defined by the American Medical Association, RPM is a digital health solution that uses connected medical devices to collect and analyze patient health data between visits to support ongoing care.
Unlike telehealth, RPM doesn’t require a live conversation. It’s focused on continuous observation through biometric data, not direct interaction.
RPM is most commonly used in chronic disease management, including:
- Hypertension
- Diabetes
- Heart disease
- COPD
Patients use cellular-connected devices like blood pressure monitors, glucose meters, or pulse oximeters, and readings are sent automatically to a provider dashboard. This enables care teams to monitor trends, identify risk early, and intervene when needed, without waiting for the next appointment.
RPM vs. Telehealth: Key Differences
Here’s a side-by-side comparison to highlight the key differences between telehealth and remote patient monitoring across core categories:
| Category | Telehealth | Remote patient monitoring (RPM) |
| Interaction type | Synchronous (real-time video or phone visits) | Asynchronous (data sent without live interaction) |
| Primary function | Consultations, behavioral health, follow-ups | Ongoing monitoring of chronic or post-acute conditions |
| Technology used | Video platforms, secure messaging tools | Connected medical devices (e.g., BP monitors, glucose meters) |
| Patient role | Active participant in live sessions | Uses device; data is transmitted automatically |
| Type of data | Subjective (self-reported symptoms and dialogue) | Objective (device-recorded biometric data) |
| Billing codes | Telehealth CPT codes (e.g., 99421–99423) | RPM CPT codes (99453–99458) |
As shown above, the two models differ not only in how care is delivered, but also in how data is collected, interpreted, and reimbursed.
Benefits of Telehealth and Remote Patient Monitoring (RPM)
Both RPM and Telehealth offer distinct benefits based on how and when care is delivered. Understanding the advantages of each can help healthcare providers choose the right approach for specific patient needs and, in many cases, use both together for more comprehensive care.
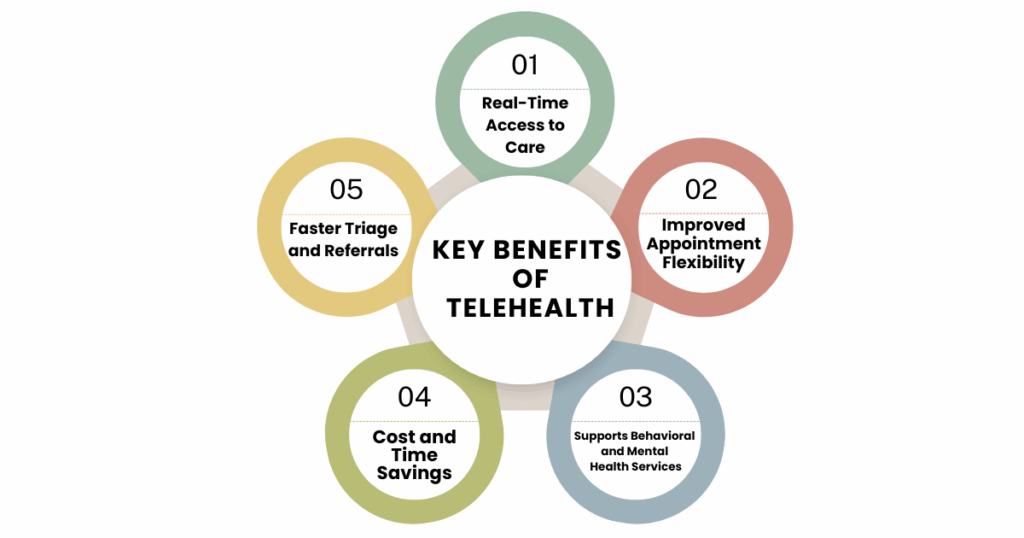
Key Benefits of Telehealth
Real-Time Access to Care
Telehealth enables live, two-way communication between providers and patients, eliminating the need for in-person visits. This improves access for patients in rural areas, those with limited mobility, or individuals needing urgent but non-emergency care.
Improved Appointment Flexibility
Providers can manage follow-ups, behavioral health check-ins, and medication reviews without requiring patients to travel. This reduces appointment cancellations and supports better continuity of care.
Supports Behavioral and Mental Health Services
Telehealth has become a widely accepted channel for delivering therapy, counseling, and psychiatric evaluations, increasing privacy and accessibility for patients.
Cost and Time Savings
Virtual visits reduce overhead for clinics and transportation costs for patients, resulting in time and financial efficiencies for both sides.
Faster Triage and Referrals
Telehealth enables quick assessment of symptoms, helping providers determine whether in-person care, testing, or emergency attention is needed.
Benefits of Remote Patient Monitoring (RPM)
Continuous, Data-Driven Care
RPM collects biometric data between appointments, providing providers with ongoing insight into a patient’s health status. This allows for faster detection of changes and more proactive intervention.
Improved Chronic Disease Management
For patients with conditions like hypertension, diabetes, and heart disease, RPM supports tighter control by tracking trends and enabling timely medication or lifestyle adjustments.
Reduced Hospital Admissions
By identifying early warning signs, RPM can help prevent complications that lead to ER visits or hospitalizations, especially for high-risk patients.
Increased Patient Engagement
Patients using home monitoring devices often become more aware of their health and more compliant with their care plans, fostering stronger provider-patient collaboration.
Revenue Potential for Healthcare Providers
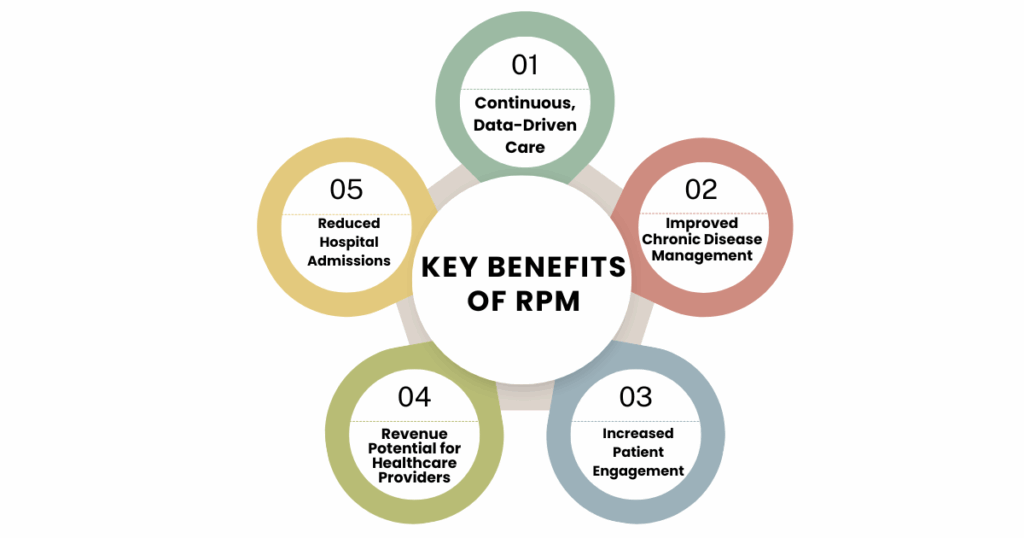
RPM is supported by dedicated CPT codes (99453–99458), allowing providers to generate ongoing revenue by billing for services such as device setup, data review, and remote patient evaluations. This not only enhances care delivery but also creates a sustainable income stream for practices adopting virtual care models.
Telehealth, Telemedicine, and Remote Patient Monitoring: What’s the Hierarchy?
These terms are often confused, so let’s clarify how they relate:
Telehealth is the broadest term. It includes any health-related service delivered using telecommunications, whether clinical, educational, or administrative.
Telemedicine is a subset of telehealth focused strictly on clinical services like diagnosis, consultations, and treatment delivered remotely.
Remote Patient Monitoring (RPM) is another subset of telehealth, but instead of live interaction, it relies on connected medical devices that collect and transmit patient data on a regular basis.
While all three use technology to bridge the gap between patients and providers, RPM is unique in its focus on ongoing, automated monitoring through connected devices.
Final Thoughts
Telehealth and Remote Patient Monitoring aren’t interchangeable, they’re interdependent. While telehealth excels at face-to-face virtual consultations, RPM provides continuous insight that’s essential for managing long-term health conditions.
Telehealth delivers care at the moment. RPM tracks patient health between those moments. Together, they create a more complete, responsive care model—one that meets patients where they are, both virtually and continuously.
If you’re building an RPM program for your practice, CandiHealth helps you simplify the entire process, from setup to clinical integration.
Schedule a walkthrough today to see how our platform streamlines remote care,
Related Articles
What is Remote Patient Monitoring (RPM) and How It’s Transforming Chronic Care
Frequently Asked Questions (FAQs)
1. Is RPM a type of telehealth?
Technically, yes. RPM is a form of telehealth, but its workflow, reimbursement, and clinical use case are unique enough that it’s treated as its own category by CMS and most providers.
2. Can RPM replace telehealth?
No. RPM captures vital signs, not symptoms or patient experiences. It doesn’t replace the need for real-time conversation, it complements it.
3. Is RPM reimbursed the same way as telehealth?
Not exactly. RPM has its own CPT codes (99453–99458), and each has usage requirements around device setup, data transmission, and clinical review.
4. What is the main difference between Telehealth and Remote Patient Monitoring (RPM)?
Telehealth involves live communication, usually video or phone between a patient and provider. RPM uses connected devices to automatically send health readings to providers, without needing real-time interaction.