Remote Patient Monitoring (RPM) has become one of the fastest-growing healthcare services in the U.S. in 2025, allowing providers to improve patient outcomes and bill for their services using specific codes.
But as RPM adoption increases, so does payer scrutiny, and documentation requirements are now a major reason for claims denial.
In this guide, you’ll learn:
- Remote Patient Monitoring documentation requirements that apply to all codes
- Specific documentation requirements for each CPT code (99453, 99454, 99457, 99458, and 99091)
- Practical checklists and templates you can use in your EHR
- Common mistakes in RPM documentation and how to avoid them
Table of Contents
Remote Patient Monitoring Documentation Requirements
In April 2025, CMS published the MLN901705 “Telehealth & Remote Patient Monitoring” guidance, updating RPM rules under the 2025 Physician Fee Schedule. This booklet confirms that RPM‑specific flexibilities remain in place, and describes documentation requirements to meet compliance and reimbursement standards
Below is a list of remote patient monitoring documentation requirements that healthcare providers need to know in 2025.
- The Healthcare provider must have an established relationship with the patient before starting RPM service.
- Document verbal or written consent before services begin.
- Use a device that meets the FDA’s definition of a medical device and automatically uploads data.
- The device must transmit data automatically. Manual entry by the patient does not qualify.
- For CPT 99454, the patient must record at least 16 days of readings in a 30-day period.
- Only one provider can bill RPM for a patient in a 30-day cycle.
- General supervision is allowed, meaning clinical staff can perform RPM services under a provider’s direction.
- For 99457/99458, document the time spent and details of real-time communication with the patient.
Documentation Requirements for Each Remote Patient Monitoring CPT Code
Here is a breakdown of the documentation requirements for each CPT code in 2025 so your claims are complete and audit-ready.
CPT 99453 Documentation Requirements
The Healthcare provider must document the following things to be eligible for Code 99453 reimbursement:
- Date RPM services began.
- Confirmation that patient consent was obtained.
- Device name/model and confirmation it meets FDA definition.
- Proof that setup and patient education were completed.
Include details of who provided the education, what was covered, and patient understanding.
CPT 99454 Documentation Requirements
You must have the proof of following to be eligible for CPT code 99454:
- Device name/model and confirmation it meets FDA requirements.
- Proof of continuous data transmission.
- At least 16 days of readings in a 30-day period.
- Device serial number or unique identifier.
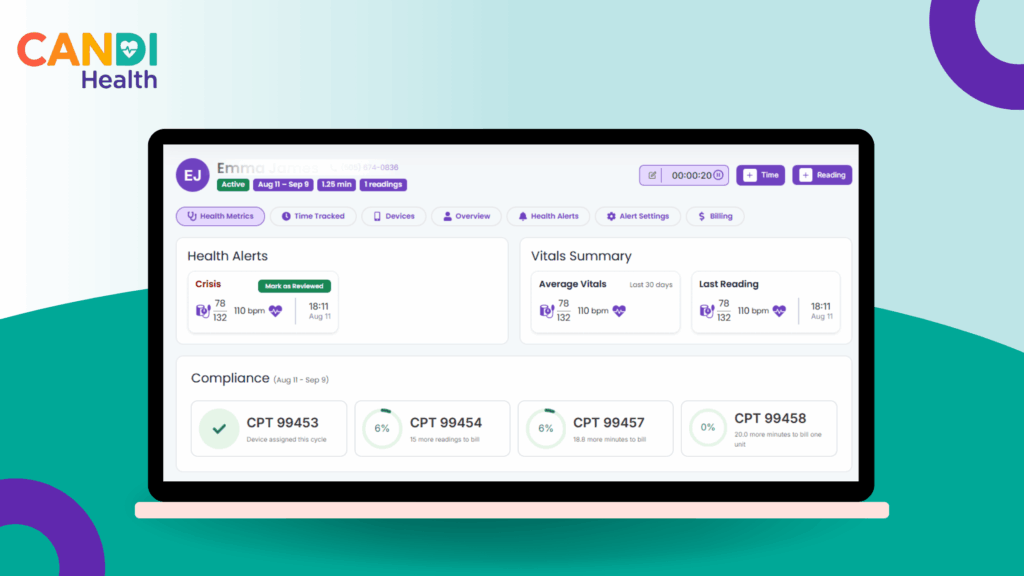
Tip: Save automated device logs or dashboard screenshots as proof of data transmission. With CandiHealth’s dashboard, you can track device status and 16-day compliance at a glance. No manual logging needed.
CPT 99457 Documentation Requirements
To be eligible for CPT code 99457 reimbursement, you must have proof of the following:
- Date(s) and time spent providing care management.
- Interactive communication details with patient/caregiver.
- Clinical decisions, care plan changes, or actions taken based on RPM data.
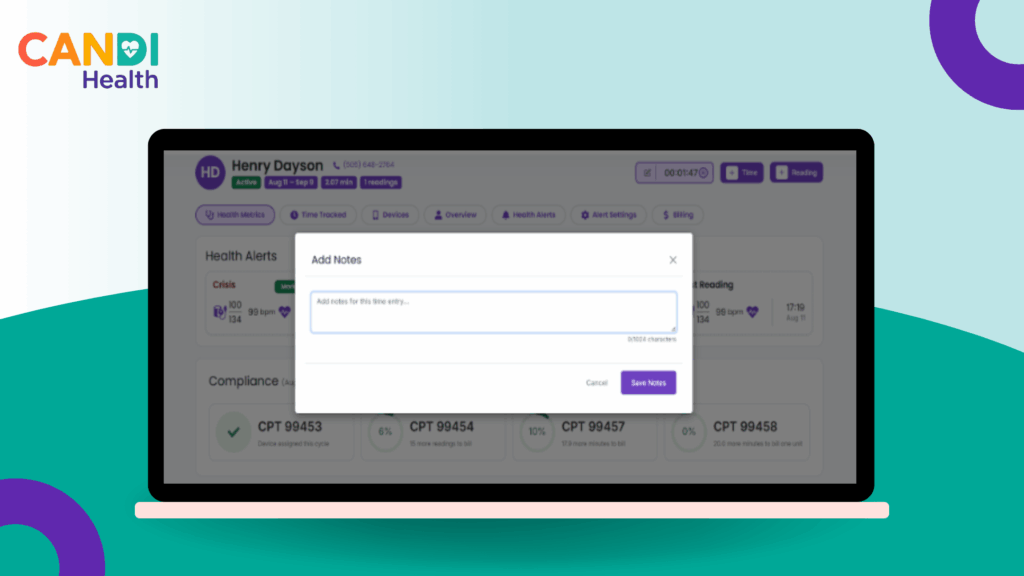
Tip: The 16-day rule does not apply — but you must show at least 20 minutes of documented time. CandiHealth automatically tracks time spent on patient care and also allows doctors to add notes, making 99457 billing audit-ready.
CPT 99458 Documentation Requirements
Document the following to be eligible for CPT code 99458 reimbursement:
- Additional 20-minute time block(s) beyond the first 20 minutes.
- Communication details and clinical actions taken.
Tip: Clearly separate time entries for 99457 and 99458 to avoid double-counting. CandiHealth’s time tracking tools help you log each block separately so you never miss a reimbursement opportunity.
Best Practices for Remote Patient Monitoring Documentation (2025)
Following Medicare’s 2025 RPM documentation requirements is essential, but going beyond the basics can make your program more efficient, compliant, and audit-ready.
1. Standardize Your Documentation Templates
Use pre-built EHR templates for each CPT code to ensure all required elements are captured every time. Include fields for consent, device details, time tracking, and clinical actions.
2. Automate Where Possible
Use RPM software that auto-records data transmission, time spent, and patient communications. Automation reduces human error and saves staff time.
3. Keep Documentation in One Place
Store all RPM records including consent forms, device specs, logs, and time entries, in a single patient file. This makes audits faster and avoids lost records.
4. Document Clinical Relevance
Don’t just note that you reviewed data; explain how it influenced care decisions. This demonstrates medical necessity, which is crucial for compliance.
5. Review for Overlap and Conflicts
Check for conflicts with other care management codes (CCM, PCM, TCM, BHI). Avoid billing errors that lead to denials or repayment requests.
Platforms like CandiHealth offer built-in compliance dashboard, ensuring every minute you spend meets payer requirements without extra administrative work.
Remote Patient Monitoring Compliance FAQs
Here are some of the most common questions asked by healthcare providers:
Q: Can CPT 99453 be billed more than once if a device is replaced?
99453 is generally billed a single time for patient onboarding and education. You may bill it again only if a completely new type of device is issued and the patient requires fresh training. Simply swapping out a broken unit for the same model does not qualify.
Q: How often can CPT 99454 be billed?
This is a recurring monthly code that covers supplying the device and daily data transmission. It is billed every 30 days, provided that at least 16 days of readings are recorded during that cycle.
Q: What if the patient doesn’t reach 16 days of readings?
If fewer than 16 days of data are recorded in the 30-day period, 99454 cannot be billed. However, 99457 can still be billed if at least 20 minutes of RPM care management is completed, including one live interaction.
Q: Is there an exception for February since it has only 28 days?
No, the 16-day requirement applies to any rolling 30-day cycle, regardless of the month’s length. February is treated the same as any other month for billing purposes.
Q: What qualifies as interactive communication?
Interactive communication refers to a live phone or video call between the provider and the patient or their caregiver. Emails, text messages, or voicemails do not meet this requirement.
Q: Do all 20 minutes need to be spent on interactive communication?
No. The 20-minute requirement includes overall care management time, but there must be at least one live conversation to bill for 99457. Additional 20-minute blocks can be billed under 99458.
Q: Can 99457 and 99458 be billed if the patient has fewer than 16 days of readings?
Yes. The 16-day rule applies only to 99454. If time and communication requirements are met, these codes can still be billed even if the 16-day threshold is not reached.
Q: Do RPM codes follow calendar months or rolling time frames?
Here is the billing frequencies of each code:
- 99453: One-time per patient per episode of care
- 99454: Every rolling 30-day cycle
- 99457/99458: Calendar month
Q: What should be included in time logs?
Time logs should clearly state how the time was used, including any patient communication, care plan updates, and notes on patient progress.
Q: Can vendor-employed staff provide RPM services?
Yes, clinical staff working under the direct supervision of the billing provider may deliver RPM services, but the billing must be submitted under that provider’s NPI.
Q: Can patients manually enter readings for RPM billing?
No, for RPM services to be billable, the device must automatically transmit data to the provider. Self-reported or manually entered readings are not eligible.
Final Thoughts
Meeting Medicare’s 2025 Remote Patient Monitoring documentation requirements protect your revenue, avoid denials, and ensure accurate patient care records. Proper documentation shows that the service was necessary, delivered correctly, and meets every requirement tied to the CPT code you’re billing. The practices that thrive under these new rules are the ones that treat documentation as a built-in process, not an afterthought.
If you’re still relying on manual spreadsheets or scattered notes, now’s the time to tighten up your workflow.
Ready to make compliance effortless? Book a demo with CandiHealth and see how automated tracking, built-in documentation, and audit-ready reports can protect your revenue.