Did you know many clinics missed out on Medicare reimbursement in 2024 simply because they didn’t bill Remote Patient Monitoring (RPM) codes correctly?
As RPM becomes a standard part of chronic care, billing it accurately has never been more important. Providers are already investing time, devices, and staff into delivering RPM, but without the right use of CPT codes, that work often goes unpaid.
The challenge isn’t just understanding what RPM is. It’s knowing which services qualify, which codes apply, and how to meet CMS documentation requirements in 2025.
This guide gives you a clear, practical breakdown of RPM CPT codes, how they work, and how to use them. Whether you’re overseeing billing, clinical workflows, or both, this is the clarity you need.
Let’s begin with the foundation: what makes RPM billable, and how CMS defines the rules.
Table of Contents
RPM Billing Fundamentals
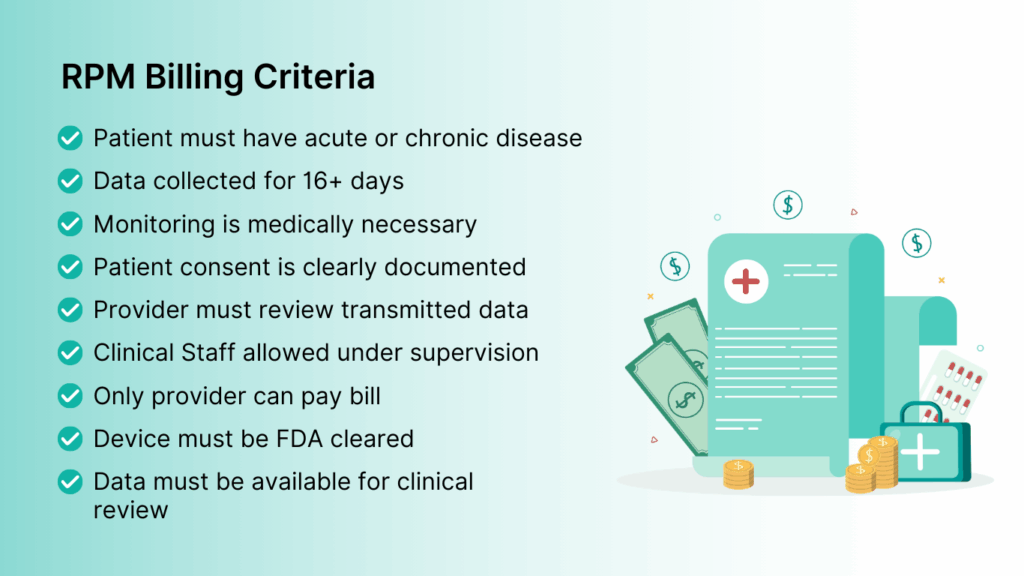
Before you bill for Remote Patient Monitoring, you need to know what actually qualifies as RPM care. Centers for Medicare & Medicaid Services (CMS) has outlined specific requirements, and missing even one can turn a claim into a denial.
Here’s what you need to know before billing any CPT code.
What Qualifies as Billable Remote Patient Monitoring in 2025
To bill RPM services, your care delivery must meet all of the following conditions:
- The patient must have an acute or chronic condition.
- Data must be collected for at least 16 days in a 30-day period.
- Only one practitioner can bill RPM per patient per 30-day period.
- Monitoring must be medically reasonable and necessary.
- The device must meet FDA definition as a medical device.
- Patient consent must be obtained at the time services begin and should be documented in the medical record.
- RPM cannot be billed with RTM for the same patient.
- Data must be accessible for clinical review and interpretation.
- Clinical staff may help deliver services as long as the billing provider maintains oversight.
RPM billing starts with qualifying care. Make sure you choose the right device, document consent, and your clinical team is actively reviewing and acting on the data.
Source: MLN901705 – Telehealth & Remote Patient Monitoring
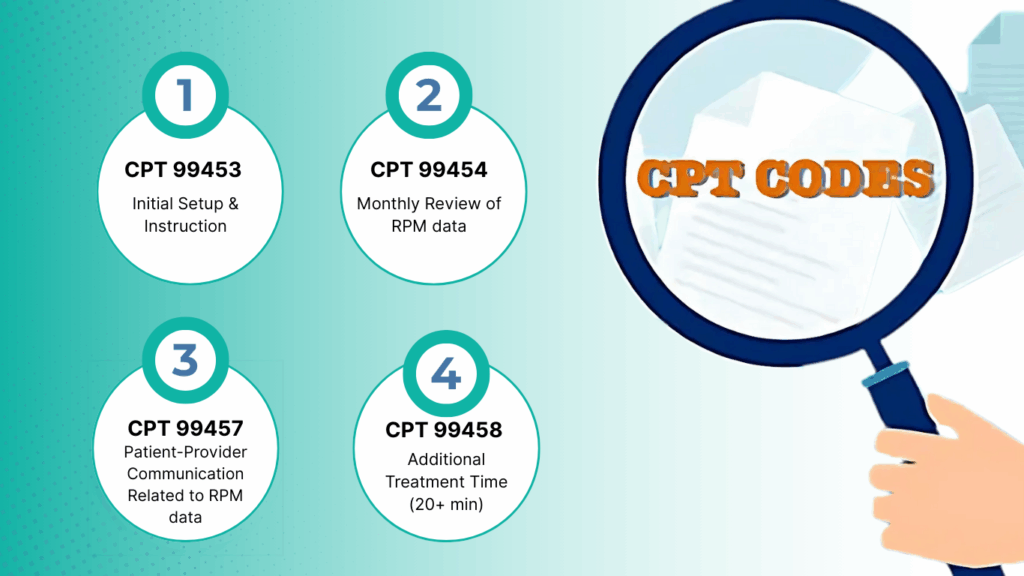
RPM CPT Codes Overview
Once the foundational requirements are in place, the next step is knowing which CPT codes apply to which part of the RPM service. CMS uses four main codes to cover the different components of Remote Patient Monitoring.
- CPT 99453 (Initial Setup & Instruction)
- CPT 99454 (Monthly Review of RPM data)
- CPT 99457 (Patient-Provider Communication Related to RPM data)
- CPT 99458 (Additional Treatment Time (20+ min)
Each code represents a distinct billable action, and correct usage is key to getting reimbursed accurately.
Below is a detailed breakdown of RPM billing codes, what it covers, how often it can be billed, and what providers need to document in 2025.
1. CPT 99453 (Initial Setup & Instruction)
This code covers the initial work involved in setting up a patient with RPM. It includes preparing the device, walking the patient through how to use it, and ensuring everything is transmitting correctly.
You can bill 99453 once per episode of care, and it must be tied to a real clinical use case. Only a physician or qualified healthcare provider can bill this code, and services may be furnished by clinical staff under general supervision.
To stay compliant, document the setup date, the provider involved, and confirmation that the patient received training.
2. CPT 99454 (Monthly Review of RPM data)
CPT 99454 is billed monthly for supplying the RPM device and collecting transmitted data. The requirement here is strict: the device must collect data for at least 16 separate days within a 30-day billing period. Anything less, and you lose billing eligibility for that month.
CMS also specifies that the device must be an FDA-defined medical device capable of automatically transmitting data. Only one provider may bill 99454 per patient, per 30-day period.
Be sure to retain logs showing transmission dates and device type in the patient record.
3. CPT 99457 (Patient-Provider Communication Related to RPM data)
This code reflects the clinical side of RPM, the time spent reviewing patient data, making decisions, and communicating with the patient.
To bill 99457, a provider or supervised clinical staff must spend at least 20 minutes in a calendar month on data-driven treatment management. Keep track of time spent, summaries of the review, and notes from any patient communication.
4. CPT 99458 (Additional Treatment Time)
CPT 99458 is used for each additional 20 minutes of RPM-related clinical activity in a calendar month, beyond the initial time billed under 99457. It reflects continued physician interpretation and communication with the patient or caregiver.
This time may include both synchronous, real-time interactions, like video or phone calls, and non-face-to-face care management services, such as reviewing trends, adjusting care plans, or coordinating with other members of the care team.
Source: Remote Patient Monitoring Billing, Coding and Regulations Information
Examples of Different RPM Billing Scenarios for Better Understanding
Knowing the rules is one thing, applying them in actual practice is where it often gets tricky. Different patient types, staffing setups, and device usage patterns can affect how and when you bill RPM CPT codes. Below are a few common scenarios that illustrate how these codes are applied in real clinical workflows.
Scenario 1: A Hypertensive Patient with Routine Monitoring
A primary care clinic sets up a patient diagnosed with hypertension on an FDA-approved Bluetooth blood pressure monitor. The medical assistant walks the patient through device setup, confirming data transmission and documenting consent.
Over the next 30 days, the patient records BP readings at least 20 times. The care team logs 24 minutes of total review time, which includes a follow-up phone call to discuss a medication adjustment.
Codes billed:
- 99453 (one-time device setup and education)
- 99454 (device supply + 16+ days of data)
- 99457 (20 minutes of treatment management including live interaction)
Scenario 2: A High-Need Diabetic Patient with Extended Follow-Up
A diabetic patient with recent complications is enrolled in RPM using a continuous glucose monitor. Throughout the month, the patient’s data is transmitted daily. The nurse practitioner reviews readings weekly and calls the patient multiple times to adjust insulin dosage.
Total documented time spent across the month is 48 minutes, with at least two of those check-ins conducted via video call.
Codes billed:
- 99453 (initial setup and training)
- 99454 (data transmission met 16-day rule)
- 99457 (first 20 minutes of clinical review + interaction)
- 99458 (additional 20 minutes of care management)
Scenario 3: Missed Threshold for Data Transmission
A patient with heart failure is provided a weight scale to monitor fluid retention. Due to travel and missed check-ins, the patient only transmits 11 readings in the billing month.
Even though the care team spent 30 minutes reviewing the case, CPT 99454 cannot be billed because the 16-day minimum wasn’t met. However, time spent on data review and care communication can still qualify for 99457.
Codes billed:
- 99457 (treatment management based on available data)
- 99454 — Not billed (threshold not met)
Scenario 4: Delegated Care Team Workflow with Supervision
A cardiology practice has a nurse-led RPM program. Clinical staff handle onboarding, device troubleshooting, and patient follow-up under the supervision of the cardiologist. The provider only steps in for medication changes and final review.
As long as general supervision is in place and time is tracked accurately, all RPM codes may still be billed by the supervising physician.
Codes billed:
All applicable CPT codes (99453, 99454, 99457, 99458) based on activity, billed under the provider’s NPI with documentation of supervisory oversight.
These scenarios highlight the importance of documentation, time tracking, and meeting minimum thresholds.
Common RPM Billing Challenges and How to Avoid Them in 2025
Billing for Remote Patient Monitoring comes with details that are easy to miss. Even when care is delivered correctly, small oversights, like missing time logs or using the wrong device, can delay claims or lead to denials.
Most of these issues are preventable with the right checks in place. Below are common RPM billing challenges and how to avoid them in day-to-day practice.
1. Missing the 16-Day Data Requirement
The most frequent billing issue happens with CPT 99454. If the patient doesn’t transmit data for at least 16 days in the 30-day period, you can’t bill for that month. This is especially common with new patients who forget to use the device consistently.
How to avoid it:
Set up automated reminders or follow-up protocols to ensure patients are using the device as expected. Consider weekly check-ins during the first month to build the habit.
2. Under-documenting Time for 99457 and 99458
Incomplete time logs or vague notes can lead to claim rejections, especially for 99458, which requires detailed justification for additional time.
How to avoid it:
Use your EHR or RPM platform to track cumulative time each month. For example, platforms like CandiHealth automatically track the time spent by a provider inside the patient profile and allow clinicians to add notes tied to each reading.
3. Billing Multiple Providers for the Same Patient
RPM codes can only be billed by one provider per patient per calendar month. When more than one clinic or specialist tries to bill RPM for the same patient, CMS typically pays the first claim and denies the rest.
How to avoid it:
Coordinate RPM enrollment across providers, especially in multi-specialty practices. Make sure the billing team checks for existing RPM activity before initiating a new program.
4. Using Non-Compliant Devices
Some clinics unknowingly use consumer health gadgets that don’t meet FDA definitions as medical devices. These may work for patient monitoring, but they won’t qualify for reimbursement.
How to avoid it:
Only use RPM devices that are FDA-cleared and capable of automatic data transmission. Store documentation on each device’s compliance status.
5. Lack of Internal Training
Even small misunderstandings—like confusing the calendar month billing period or misidentifying who can supervise RPM, can lead to errors that delay claims.
How to avoid it:
Train both clinical and billing teams on current CMS requirements. Keep updated documentation and hold periodic reviews to catch mistakes before they go out the door.
Many of the challenges outlined above; missed time tracking, incomplete documentation, or inconsistent data logging, can be avoided with the right tools in place.
CandiHealth’s platform automatically tracks provider time, timestamps clinical notes, and ties each action to the patient record. It simplifies compliance so your team can focus on care, not paperwork.
Related Articles
What is Remote Patient Monitoring (RPM) and How It’s Transforming Chronic Care
Frequently Asked Questions (FAQs)
1. Can I bill RPM for a patient who only transmitted data for 10 days?
No. To bill CPT 99454, the patient must transmit physiological data for at least 16 days within a 30-day period. If this threshold isn’t met, the code cannot be billed—even if care was provided.
2. Does 99457 require real-time communication with the patient?
Yes. 99457 requires at least one live, interactive communication with the patient or caregiver (e.g., a phone or video call). Texts, portal messages, or voicemails do not meet the requirement.
3. Can clinical staff provide RPM services under general supervision?
Yes. Clinical staff can deliver RPM services—like setup and care management—under general supervision of a physician or qualified practitioner. The supervising provider remains responsible for billing and documentation.
4. Can multiple providers bill RPM for the same patient in the same month?
No. Only one provider can bill RPM services per patient in a calendar month. If multiple claims are submitted, only the first will typically be reimbursed.
5. Do I need written consent to bill RPM?
Not necessarily. Verbal consent is acceptable under CMS guidelines, but it must be documented in the medical record. Some providers still prefer written consent for added clarity during audits.
Final Thoughts
Remote Patient Monitoring creates space for proactive care, better outcomes, and sustainable revenue. But delivering RPM successfully means more than using the right devices. It means using the right codes, documenting each step, and aligning every action with CMS expectations.
With a clear workflow, accurate time tracking, and a reliable platform like CandiHealth, your team can bill confidently and stay audit-ready.
Want to make your RPM program easier to manage?
Get in touch with our team or explore how CandiHealth can support your workflow—accurately, efficiently, and without the guesswork.