Starting a Remote Patient Monitoring (RPM) program can feel overwhelming. The devices, the billing codes, the legal requirements; it’s a lot to take in, especially when you’re already managing a full patient load. But here’s the truth: launching RPM at your clinic doesn’t have to be complicated.
With the right steps and support, you can build a simple, compliant RPM program that improves patient outcomes and creates a new revenue stream, without adding extra burden to your staff.
Learn how to start or launch an RPM program at your clinic step-by-step in this guide.
Table of Contents
What Is a Remote Patient Monitoring (RPM) Program?
Remote Patient Monitoring (RPM) allows healthcare providers to track their patients’ health while they’re at home, without needing them to visit your clinic. Patients use simple, FDA-approved devices like blood pressure monitors, glucose meters, or weight scales. RPM devices then transmit data automatically to the doctor’s clinical dashboard.
So, what’s the difference between telehealth and RPM?
RPM is not the same as telehealth. Telehealth involves live video calls. RPM, on the other hand, collects health data continuously in the background, helping doctors catch problems early and take timely action.
RPM helps providers stay connected with patients suffering from chronic conditions like hypertension, diabetes, or heart failure.
Why Should You Start an RPM Program?
Here are the top benefits of starting an RPM program for your clinic:
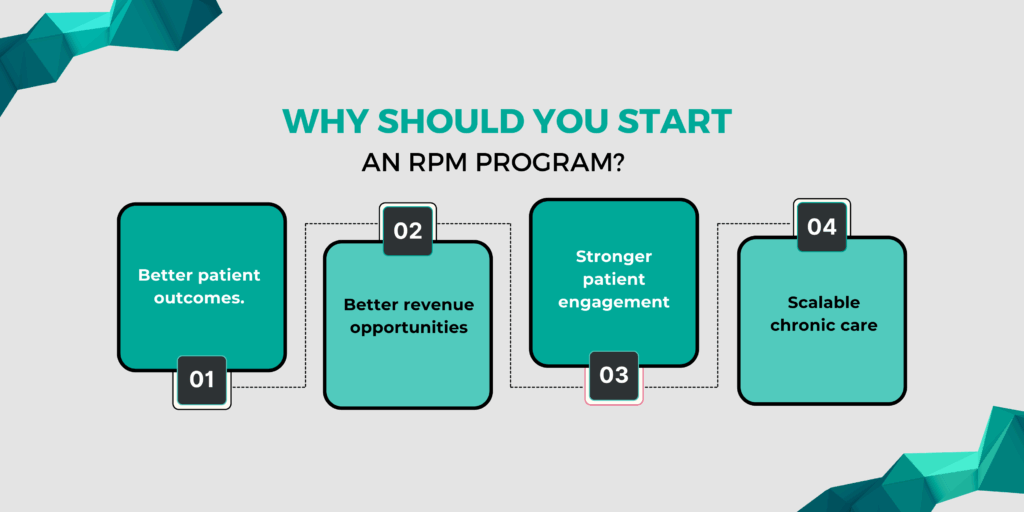
- Better patient outcomes.
- Better revenue opportunities
- Stronger patient engagement
- Scalable chronic care
Here is a brief overview of each benefit.
1. Better Patient Outcomes
RPM gives you regular updates on your patients’ vitals, even when they’re not in your clinic. This helps you catch problems early, before they become emergencies. You can adjust treatment plans in real time, leading to better control of chronic conditions like hypertension, diabetes, and heart failure.
2. Better Revenue Opportunities
RPM services are covered by Medicare and many private insurers. With proper documentation and time tracking, you can bill for setup, device supply, and monthly monitoring using CPT codes like 99453, 99454, 99457, and 99458. Many clinics generate $100–$150 per patient per month, making RPM a reliable source of recurring income.
3. Stronger Patient Engagement
When patients track their own health and know their data is being reviewed, they become more involved in their care. RPM builds trust and makes them feel supported between appointments.
4. Scalable Chronic Care
Whether you have 10 or 100 chronic care patients, RPM helps you manage them efficiently without adding pressure to your schedule. Alerts can be prioritized, and care coordinators or nurses can handle routine reviews, giving you time for higher-risk patients.
Is Your Practice Ready for RPM?
Before launching a Remote Patient Monitoring (RPM) program, it’s important to make sure your clinic is ready to support it—clinically, operationally, and financially. Here’s a quick readiness checklist to help you decide before implementing RPM program for your clinic:
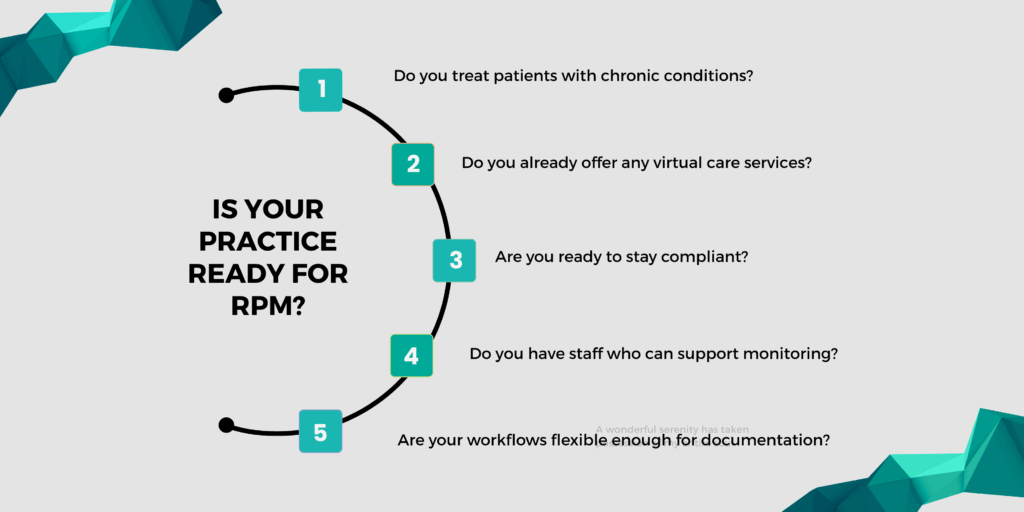
1. Do you treat patients with chronic conditions?
RPM works best for patients with ongoing health issues like hypertension, diabetes, heart disease, or COPD. If a large part of your patient population falls into these categories, you’re in a good position to benefit from RPM.
2. Do you already offer any virtual care services?
If your clinic has used telehealth or other digital tools, you’re likely familiar with the basics of remote workflows. That experience can make it easier to integrate RPM into your daily routine.
3. Do you have staff who can support monitoring?
RPM doesn’t require hiring new staff, but someone on your team, such as a nurse or care coordinator should be able to handle daily data reviews, highlight alerts, and follow up with patients. Clear roles and communication are key to running a smooth program.
4. Are your workflows flexible enough for documentation?
RPM billing requires accurate time tracking, consent documentation, and consistent note-keeping. If your clinic uses an EHR system or structured documentation process, you’re already one step ahead.
5. Are you ready to stay compliant?
HIPAA compliance and data security are essential. Make sure any devices and platforms you use are secure, and your staff understands how to handle patient data properly.
Quick RPM Readiness Score:
- 4–5 Yeses? You’re ready to get started.
- 2–3 Yeses? You’re close—some minor planning can fill the gaps.
- 0–1 Yes? Consider partnering with an RPM vendor to simplify the setup.
How to Start an RPM Program in 2025: Step-by-Step Process
You don’t need a large team or complicated systems to launch a Remote Patient Monitoring (RPM) program. Follow these steps to build a compliant, efficient workflow that improves care and drives new revenue for your clinic.
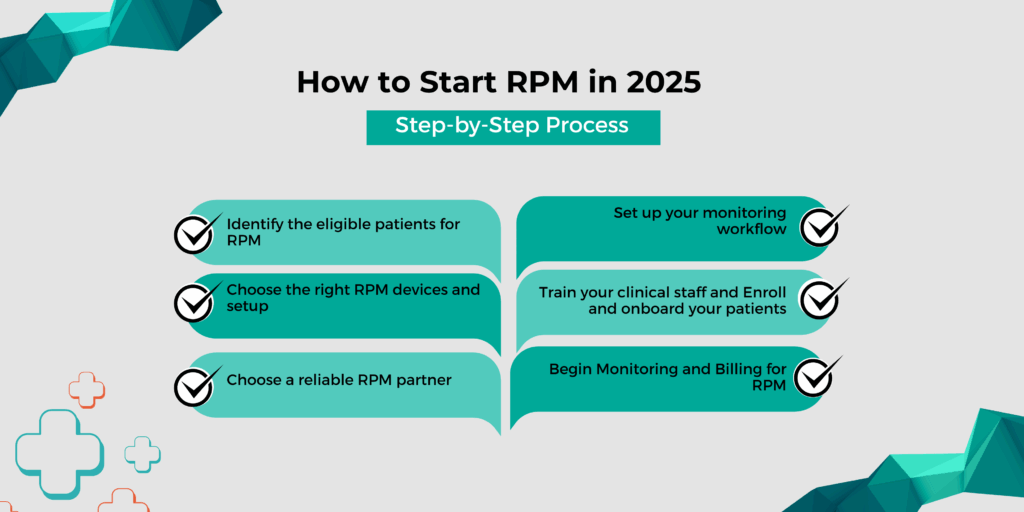
- Identify the eligible patients for RPM
- Choose the right RPM devices and setup
- Choose a reliable RPM partner
- Set up your monitoring workflow
- Train your clinical staff
- Enroll and onboard your patients
- Begin Monitoring and Billing for RPM
Here is a brief overview of each step of implementing the RPM program in 2025 for your clinic.
1. Identify the Eligible Patients for RPM
Start with patients who have chronic conditions that require consistent monitoring, such as hypertension, diabetes, COPD, or heart failure. These patients are typically eligible for RPM coverage under Medicare and private insurers. To be eligible for remote patient monitoring,
- Patients must have at least one chronic condition
- Devices must be used for at least 16 days per month
- Consent must be obtained and documented
If chronic care is already a part of your daily work, RPM is a natural next step.
2. Choose the Right RPM Devices and Setup
The devices you choose can make or break your RPM program. Look for FDA-approved, cellular-enabled options that are easy for patients to use. Popular device types include:
- Blood pressure monitors
- Glucose meter
- Pulse oximeters
- Weight scales
- Spirometers (for respiratory conditions)
Why cellular devices?
They don’t require Wi-Fi or smartphone apps, which reduces setup errors and improves data reliability, especially for older or non-tech-savvy patients.
A good RPM partner like CandiHealth provides pre-configured devices that are ready to use out of the box, eliminating the need for technical setup at the clinic or at home.
Schedule your free demo CTA
3. Choose a Reliable RPM Partner
Managing RPM in-house is resource-intensive and prone to compliance issues. That’s why most practices choose to work with a specialized RPM partner who can handle:
- Device supply and shipping
- A HIPAA-compliant monitoring platform
- Support for Medicare billing workflows
- Patient onboarding tools and clinical education
- Optional staffing for monitoring and triage
What to look for in a partner:
- Are the devices cellular-enabled and FDA-cleared?
- Is the platform easy for your team to use?
- Do they help with billing and time tracking?
- Will they provide training and ongoing support?
CandiHealth offers all of the above, making it easy for your clinic to launch quickly with minimal administrative overhead. We support your entire RPM workflow, from devices to billing, so you can focus on patient care.
4. Set Up Your Monitoring Workflow
Once your platform is in place, define a clear workflow so your team knows exactly how to manage daily tasks. A good platform should provide:
- Real-time dashboards showing patient readings
- Alert systems for out-of-range data
- Time tracking tools to log billable minutes
- Customizable reports for audits and compliance
Assign roles internally. Decide who will:
- Review alerts and respond to patients
- Track time and submit billing
- Escalate high-risk cases to providers
Even small teams can run RPM smoothly with a well-defined process.
5. Train Your Clinical and Staff
Training doesn’t have to take long, but it needs to be specific. Everyone on your team should understand:
- How to review and interpret RPM data
- What counts toward billing time
- How to document patient interactions
- How to communicate with patients using RPM insights
If you partner with CandiHealth, we’ll provide your staff with quick-start guides, billing checklists, and platform training videos to get your team up to speed fast.
6. Enroll and Onboard Patients
Once your team is ready, start enrolling eligible patients. Use a simple explanation like: “We’re offering a new service that lets us monitor your health between visits using a device you use at home. You’ll use it just like you would normally, and we’ll get alerts if anything looks off, so we can adjust your care sooner.” Follow these steps to enroll your patients:
- Obtain verbal or written consent (as required)
- Deliver or ship the device to the patient
- Document the enrollment and start date
- Begin collecting data and reviewing trends
7. Begin Monitoring and Billing for RPM
With your program live, here’s how your clinic maintains it:
- Monitors patient readings regularly
- Logs interactions for time-based billing
- Responds to alerts or escalates when needed
- Submits claims using the correct RPM CPT codes:
Most clinics begin to see steady monthly revenue within the first 60 days of starting their program.
RPM Billing and Reimbursement Basics
Remote Patient Monitoring (RPM) is a reimbursable service under Medicare and many private payers. With the right documentation and workflows in place, your clinic can earn up to $100 per patient per month through RPM.
Here’s what you need to know to bill accurately and stay compliant.
Key RPM CPT Codes
These are the main billing codes used for RPM. You’ll need to apply them correctly based on what service was delivered:
| CPT Code | Description | Reimbursement Amount | Billing Frequency |
| 99453 | Initial setup and patient education | $19.73 | One-time per patient |
| 99454 | Monthly remote monitoring with daily recordings from the connected device | $43.02 | Monthly |
| 99457 | Monitoring and treatment of the patient for at least 20 minutes throughout the month | $47.87 | Monthly |
| 99458 | Each additional 20 minutes of monitoring | $38.49 | Monthly |
Note: All figures listed above are taken from the official CMS Physician Fee Schedule. You can use that tool to search CPT codes and view the latest national and regional Medicare rates.
CandiHealth tracks all billable time and documentation directly inside the platform to help reduce errors and streamline your billing process.
What Can You Expect to Earn with RPM?
Most clinics enrolled in RPM see up to $100/month per patient in reimbursement, depending on how many services are billed. Here’s a simple example:
- Setup & education (one-time): 99453 – ~$19
- Device transmission (monthly): 99454 – ~$43
- Clinical care (monthly):
- 99457 – ~$47
- 99458 – ~38 (if applicable)
Multiply that by 20, 50, or 100 patients, and RPM can quickly become a steady, scalable revenue stream for your practice.
Calculate ROI here: Estimate Your RPM Revenue Potential
What Documentation Do You Need?
To bill RPM compliantly, your clinic must track and store:
- Patient consent (verbal or written, depending on payer)
- Device usage records (must meet 16-day minimum for 99454
- Time logs for 99457/99458 showing 20+ minutes of clinical interaction
- Clinical notes summarizing care decisions, alerts, or interventions
- Staff roles involved in care (nurse, MA, physician, etc.)
All of this should be documented in your EHR or RPM platform, and readily accessible in case of audits.
Common Billing Mistakes to Avoid
Even small oversights can lead to denied claims or compliance issues. Avoid these common pitfalls:
- Billing 99454 without confirming 16+ days of device usage
- Logging time without patient interaction (99457 requires live contact)
- Missing patient consent documentation
- Stacking 99458 when time doesn’t exceed 40 total minutes
- Forgetting to document clinical decisions in response to alerts
Tip: CandiHealth automatically tracks usage, time, and CPT eligibility, reducing administrative errors and protecting your clinic from claim denials.
Final Thoughts: Start Small, Grow Smart
Don’t feel pressured to launch RPM across your entire patient base right away. It’s better to start small, get your workflow right, and scale from there. Begin with 10–15 patients who are tech-comfortable and have clear clinical needs (like uncontrolled hypertension or diabetes)
Focus on quality—document time, respond to alerts, and learn the billing process. Track outcomes and refine your workflow based on staff feedback and patient engagement.
CandiHealth makes it easy to start with a pilot program and grow as your team becomes more comfortable.
Related Articles
- What is Remote Patient Monitoring (RPM) and How It’s Transforming Chronic Care
- Telehealth vs. RPM. What’s the Difference?
- RPM CPT Codes & Reimbursement Rates
Frequently Asked Questions (FAQs)
Q1. How do I get started with RPM?
To get started with Remote Patient Monitoring (RPM), your clinic needs to:
- Identify eligible patients with chronic conditions
- Use FDA-cleared, connected devices to collect vitals
- Set up a secure platform to receive and review the data
- Train your staff on workflows, documentation, and billing
- Obtain patient consent and begin monitoring
- Bill for services using approved CPT codes like 99453, 99454, 99457, and 99458
Q2. How to start an RPM file?
“Starting an RPM file” typically means creating a patient record for RPM services. This includes:
- Documenting eligibility and clinical need
- Recording verbal or written consent
- Registering the device to the patient profile
- Tracking device usage and monitoring start date
- Logging care activities for billing
Q3. What is an RPM program?
A Remote Patient Monitoring (RPM) program allows your clinic to monitor patients’ vital signs while they’re at home, using connected medical devices. Data like blood pressure, glucose levels, or weight is sent to your clinic in real time. This helps your team catch issues early, adjust treatment faster, and stay connected between visits.
Q4. What training is needed for RPM?
Your team should be trained on:
- How to review and respond to patient data
- How to track time for billing CPT codes (99457/99458)
- How to use the monitoring platform
- How to educate and onboard patients
- How to document care interactions properly