Avoiding extra RPM fees is one of the biggest concerns for clinics running remote patient monitoring programs. On paper, the model looks simple: patients use devices, data flows to the clinic, and providers bill for the service. But in practice, small mistakes and overlooked details often lead to hidden costs.
Extra RPM charges may come from device logistics, software pricing, or billing errors. These can reduce margins and create more admin work for staff. Yet RPM is still worth the effort. When managed correctly, it improves patient outcomes, builds trust, and creates steady revenue for clinics.
This guide explains where extra RPM fees usually come from and how healthcare providers can avoid them. The goal is to help healthcare teams run RPM programs that are both effective for patients and sustainable for the practice.
What Are Extra RPM Fees and Hidden Costs?
Extra RPM fees are charges that go beyond the standard costs you expect when running a remote patient monitoring program. These can show up in many ways: vendor markups, billing mistakes, or administrative gaps. The problem is that most of these costs aren’t obvious at the start. They surface later; in invoices, denied claims, or staff overtime, and eat into the revenue clinics count on from RPM.
Some of the most common examples include:
What You Need to Understand to Avoid Extra RPM Fees
- Device markups and logistics: higher-than-expected prices for equipment, shipping, or replacements.
- Platform or software add-ons: per-patient fees, extra charges for alerts or integrations.
- Billing errors: submitting claims without proper consent or missing Medicare requirements.
- Staff time: extra hours spent tracking data, correcting claims, or handling device returns.
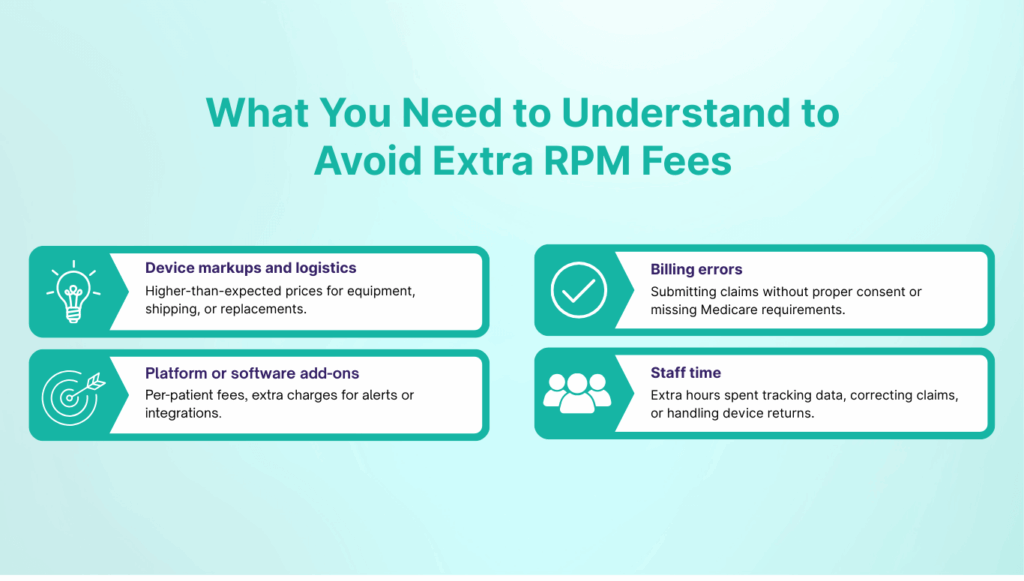
Understanding these areas is the first step. Once clinics know where hidden costs tend to appear, they can build processes to avoid them and keep RPM financially sustainable.
Estimate Your Remote Patient Monitoring (RPM) Revenue Potential
Key Components That Often Result into Extra RPM Fees
Remote patient monitoring (RPM) costs go beyond devices. Each part of the program — from hardware to billing — can create hidden fees if not managed carefully. Below are the major areas where clinics tend to overspend, with examples of how those costs show up in practice.
1. RPM Device Costs and Connectivity Fees
Devices are the backbone of any RPM program, and they’re also where many clinics see unexpected expenses. Buying devices outright feels like a one-time investment, but if patients stop using them, they sit unused and never generate revenue. Renting or leasing seems flexible, but those costs continue whether or not patients remain engaged.
The choice between Bluetooth and cellular devices matters too.
- Bluetooth devices may look cheaper upfront ($30–$100 each), but patients often need to download apps, remember log-ins, and troubleshoot connection issues. Many stop using the device altogether, leaving clinics with wasted equipment and no billable readings.
- Cellular devices cost more ($80–$200+), but transmit readings automatically. This improves adherence, reduces staff time spent on support, and helps clinics avoid losing reimbursement.
- Hidden fees may include monthly data charges, replacement costs for lost units, or shipping fees that add up across dozens of patients.
Healthcare providers must ask these questions to RPM vendors before starting an RPM program in USA:
- Is cellular connectivity included in the price, or billed separately?
- What happens if patients don’t return devices?
- Are devices covered under warranty or replacement plans?
| Device Type | Cost Range | Risks | Benefit |
| Bluetooth | $30–$100 | Patient drop-offs, troubleshooting time | Lower upfront cost |
| Cellular | $80–$200+ | Higher upfront | Higher adherence, fewer staff hours |
| Rental/Lease | $20–$40/mo | Contract lock-ins, return fees | Predictable monthly spend |
2. RPM Software and Monitoring Fees
Software costs often look small upfront but grow quickly with scale. Most vendors use one of three models: per-patient, per-provider, or revenue sharing.
- Per-patient license: $10–$40 per patient/month. A 50-patient program can add $500–$2,000/month in platform costs alone.
- Per-provider license: $100–$500 per provider/month. Some clinics get billed multiple times if more than one provider accesses the system.
- Revenue sharing: Instead of fixed fees, some vendors take a percentage of RPM reimbursement (often 20–30%). While this reduces upfront cost, clinics end up giving away part of their Medicare revenue on every claim.
- Premium support: Dedicated account managers or 24/7 service can add $500+/month.
Hidden traps: EHR integrations, analytics dashboards, or even alert notifications are sometimes billed separately. Many contracts also include automatic annual increases.
3. Vendor and Logistics Costs
Shipping, device returns, and inventory management can quietly drain budgets. Rural or overnight deliveries often add $40–$60 per shipment. When patients misplace or delay returning devices, vendors may bill the clinic for replacements. Without an inventory process, extra stock piles up unused.
Different service models shift costs in different ways:
- DIY: Cheapest upfront, but clinic staff handle logistics and training, which adds hidden workload.
- Hybrid: Vendors manage devices, while clinics handle monitoring. Balanced but still resource-heavy.
- Turnkey: Vendor manages devices, logistics, and monitoring. Easier on staff, but usually the most expensive.
4. Staff Time and Administrative Work
Some of the most overlooked RPM extra costs come from staff hours. Nurses may spend hours each week reminding patients to record readings, while billing teams often rework denied claims. Over time, this eats into care delivery and may even require hiring extra staff. Training and implementation also carry costs, from $1,000 for small practices to $10,000+ for larger groups integrating with EHRs.
For many clinics, the trade-off comes down to whether the vendor’s platform reduces workload or adds to it. Automation for reminders, compliance tracking, and billing support can save staff time — while “barebones” systems push that burden back onto the clinic.
Read more about patient compliance here: How to Increase Patient Compliance in Remote Monitoring?
5. Billing and Reimbursement Pitfalls
Billing errors remain one of the most expensive challenges in RPM. Using the wrong CPT code (e.g., 99458 instead of 99457), missing consent documentation, or failing the 16-day requirement can wipe out expected revenue.
Even when staff deliver the work, Medicare won’t reimburse if requirements aren’t met. Some vendors charge extra for compliance dashboards or audit-ready reporting, making it harder to stay on track without added costs.
Best Practices for Avoiding Extra RPM Fees
Hidden costs can’t always be eliminated, but they can be controlled with the right systems and processes. Clinics that succeed with RPM usually share a few common habits.
1. Review Vendor Contracts Carefully
Before signing, look beyond the headline numbers. Ask about:
- Device replacement policies
- Shipping and return costs
- Annual fee increases
- Support tiers (basic vs premium)
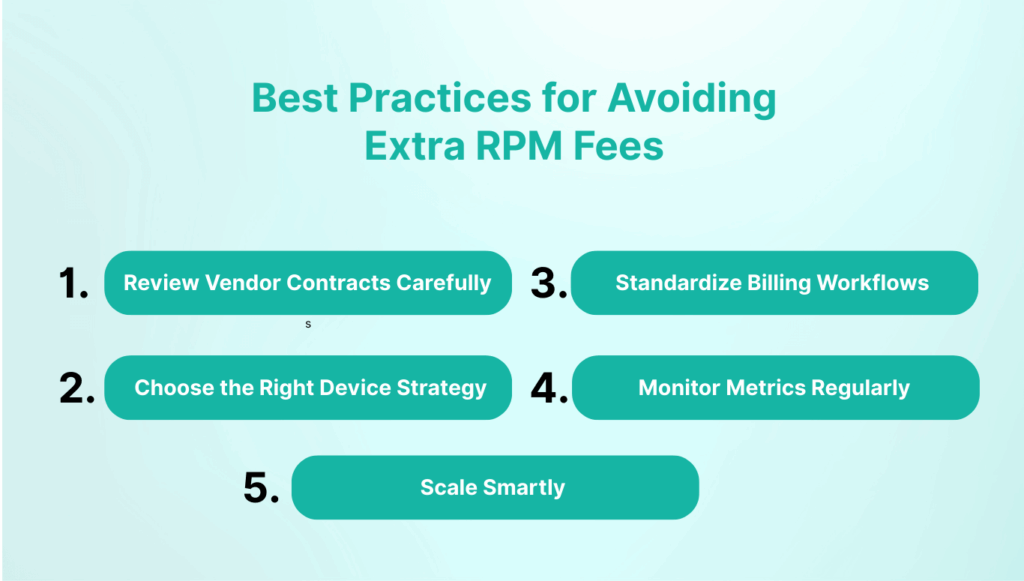
A clear contract upfront prevents surprises later.
2. Choose the Right Device Strategy
Think about your patient population. For tech-savvy patients, Bluetooth may work. For older adults or rural communities, cellular devices usually lead to better compliance and fewer drop-offs. The “cheaper” choice can cost more when patients stop transmitting readings.
3. Standardize Billing Workflows
Train staff on CPT codes and Medicare requirements. Build a checklist that includes consent capture, 16-day monitoring validation, and documentation of staff-patient interactions. Standardization reduces denials.
4. Monitor Metrics Regularly
Track usage rates, claim rejections, device returns, and staff hours. Even small variances can point to where costs are leaking. Clinics that monitor these numbers monthly are better prepared to adjust.
5. Scale Smartly
Don’t rush to enroll hundreds of patients right away. Start small, refine workflows, then expand. This way, hidden costs surface while the program is still manageable.
Key Takeaway: Avoiding extra RPM fees isn’t about cutting corners. It’s about building processes that make the program predictable and sustainable. Clinics that approach RPM with clear contracts, the right device mix, standardized billing, and ongoing monitoring tend to see stronger outcomes and more reliable revenue.
Turning Best Practices Into Reality With CandiHealth
Throughout this guide, we’ve looked at where clinics often lose money on RPM — hidden device fees, unpredictable software costs, staff burnout, and billing denials. We’ve also outlined best practices that can prevent these problems: clear contracts, patient-friendly devices, standardized billing, and audit-ready compliance.
The challenge is that most vendors don’t make this easy. Many rely on $20–$40 per patient pricing or take 20–30% of Medicare reimbursements, making it hard for clinics to scale without sacrificing margins. Others charge extra for features like compliance logs or patient reminders — things that should be built in.
CandiHealth takes a different approach. Our model is simple and predictable: $10 per patient, flat.
- No revenue-sharing.
- No surprise invoices.
- Compliance, reminders, and audit-ready tracking included.
That means clinics can project costs accurately, protect revenue, and spend less time chasing patients or fixing claims. Instead of adding complexity, CandiHealth is designed to remove it — so providers can focus on care, not costs.
What providers say:
“We used to spend more time fixing claims than running the program. With CandiHealth, billing is predictable and patients stay engaged. The flat pricing model alone has saved us thousands.” – Independent Primary Care Clinic, Texas
If you’d like to see how much your clinic could save with a flat-rate model, schedule a quick demo with our team now.
Related Articles:
Estimate Your Remote Patient Monitoring (RPM) Revenue Potential
How to Increase Patient Compliance in Remote Monitoring?
Remote Patient Monitoring Documentation Requirements (2025)
Frequently Asked Questions (FAQs)
1. What are the problems with remote patient monitoring?
Common problems include hidden costs (shipping, replacements, revenue-sharing), patient drop-offs (especially with Bluetooth devices), and billing mistakes like missing consent or failing the 16-day rule. These challenges can reduce reimbursement and increase staff workload.
2. How much does RPM cost?
Costs vary by vendor. Devices can cost $30–$200+ each or $20–$40/month to lease. Software typically ranges from $10–$40 per patient/month or $100–$500 per provider. Some vendors also use revenue-sharing models, taking 20–30% of reimbursement.
3. How to bill for remote therapeutic monitoring (RTM)?
RTM uses a different set of CPT codes (98975–98981) than RPM. It covers non-physiological data such as musculoskeletal or respiratory therapy tracking. Like RPM, providers must document consent and patient engagement to receive reimbursement.
4. Is remote patient monitoring worth it?
Yes, when managed properly. RPM improves patient outcomes, reduces hospitalizations, and generates new revenue streams for providers. The key is choosing a vendor like CandiHealth that prevents hidden costs and ensures compliance so the program remains profitable.
5. Why do RPM claims get denied?
The most common reasons are incorrect CPT coding, missing consent documentation, and failing Medicare’s 16-day requirement. Without audit-ready records, even legitimate claims may be rejected.
6. How does CandiHealth pricing work?
CandiHealth offers flat-rate pricing at $10 per patient per month. There are no revenue-sharing contracts or hidden fees. Devices are preconfigured and compliance tracking is built in, helping clinics keep costs predictable and sustainable.