Millions of Americans deal with chronic conditions like high blood pressure, diabetes, or heart disease every day. That’s why Chronic Care Management (CCM) is one of Medicare’s most important programs for doctors and patients living with these long-term health issues.
To support this, Medicare offers monthly payments to clinics and doctors who provide CCM services. The goal is simple: keep patients healthier, reduce hospital visits, and reward providers who manage care between appointments.
In this blog, you’ll learn
- How much Medicare pays for Chronic Care Management
- What billing codes you need to know
- How your clinic can make the most of these opportunities
By the end, you’ll have a clear picture of CCM reimbursement and how it can benefit both your patients and your practice.
Key Takeaways
- Medicare pays $62–$147+ per patient, per month for CCM, depending on the CPT codes used.
- Even a small panel of patients can bring in thousands of dollars each month.
- Documentation, patient engagement, and staff support are key to making CCM work smoothly.
- Combining CCM with Remote Patient Monitoring (RPM) increases both reimbursement and patient outcomes, often pushing monthly revenue per patient over $170.
What is Chronic Care Management (CCM)?
Chronic Care Management, often called CCM, is a Medicare program that pays healthcare providers for helping patients who live with more than one chronic condition. These are long-term health issues, like high blood pressure, diabetes, asthma, or arthritis, that usually last a year or more and require regular care.
CCM covers the time doctors and care teams spend managing a patient’s health outside the clinic. This includes creating a care plan, checking on medications, coordinating with specialists, and following up with patients between visits.
For clinics, CCM offers two big benefits:
- Better outcomes for patients, because care is more consistent and connected.
- Monthly Medicare payments which create a steady stream of revenue.
In simple terms, CCM is Medicare’s way of making sure providers are rewarded for the real work that happens between office visits.
How Much Does Medicare Pay for Chronic Care Management?
Many healthcare providers in the US often ask this question. But the answer depends on a few important parts. Medicare sets specific rules for CCM and uses billing codes to pay clinics per month. To understand the process simply, let’s break it down into three parts:
- Medicare Coverage Basics (You’ll learn who qualifies for CCM and what is required).
- Reimbursement Rates (Understand the exact CPT codes and how much they pay).
- How to Maximize Payments (Learn tips for making CCM more effective and profitable).
By understanding each part, you can see both the financial opportunity and the patient care benefits that CCM provides.
1. Medicare Coverage Basics
Medicare only pays for Chronic Care Management (CCM) when certain conditions are met. This ensures that the program is used for patients who truly need ongoing support.
Eligibility Rules for CCM
- The patient must have two or more chronic conditions.
- These conditions must be expected to last 12 months or longer.
- The conditions must place the patient at significant risk of decline or death if not managed.
- The patient must give consent (verbal or written) to enroll in CCM.
To make this easier, here’s a quick view:
| Requirement | What It Means | Example |
| 2+ Chronic Conditions | Patient must have at least two long-term conditions | Diabetes + Hypertension |
| Lasts 12+ Months | Conditions are ongoing, not short-term | Arthritis, COPD |
| Risk of Decline | Conditions could worsen without management | Heart Disease |
| Patient Consent | Patient agrees to receive CCM services | Signed or verbal agreement |
Providers must also create a comprehensive care plan and document all time spent managing the patient’s health outside of office visits.
This coverage framework sets the stage for how much Medicare pays, which we’ll explain next when we look at the specific CPT codes and reimbursement rates.
2. Reimbursement Rates & CPT Codes
Medicare pays for Chronic Care Management (CCM) using specific CPT codes. Each code reflects the type of service provided and the time a care team spends managing a patient’s health outside clinic. These codes help providers get reimbursed for the important work of care planning, medication management, and ongoing patient support.
Here’s a breakdown of the most common CCM CPT codes and their 2025 national average Medicare payments. These rates often vary based on specific location or payer contract.
| CPT Code | Description | Average 2025 Medicare Payment | Who Provides the Service |
| 99490 | 20 minutes of non-complex CCM in a month | ~$62 per patient/month | Clinical staff under physician/NP/PA supervision |
| 99439 | Each additional 20 minutes of non-complex CCM | ~$47 per patient/month | Clinical staff |
| 99491 | 30+ minutes of CCM personally by a physician/NP/PA | ~$85 per patient/month | Physician, NP, or PA |
| 99437 | Each additional 30 minutes of provider time | ~$60 per patient/month | Physician, NP, or PA |
Example of Monthly Reimbursement
If a clinic manages 100 Medicare patients under CPT 99490 (the base CCM code), the monthly revenue could be:
100 patients × $62 = $6,200 per month (over $74,000 per year).
If those same patients require extra time (billed under CPT 99439), the revenue potential increases even further.
Why This Matters for Clinics
- CCM creates a steady monthly income stream for providers.
- Payments are per patient, per month, making revenue predictable.
- Clinics that combine CCM with Remote Patient Monitoring (RPM) can earn even more, since Medicare allows billing for both programs when requirements are met.
In short, Medicare pays between $62 and $147+ per patient each month depending on the codes used, which adds up quickly when scaled across dozens or hundreds of patients.
How Can Clinics Maximize Reimbursements?
To truly benefit from Medicare’s Chronic Care Management (CCM) program, clinics need to manage their processes carefully. Many providers miss out on revenue because of incomplete documentation, staff overload, or lack of patient engagement. With the right strategies, you can capture the full reimbursement and improve patient outcomes at the same time.
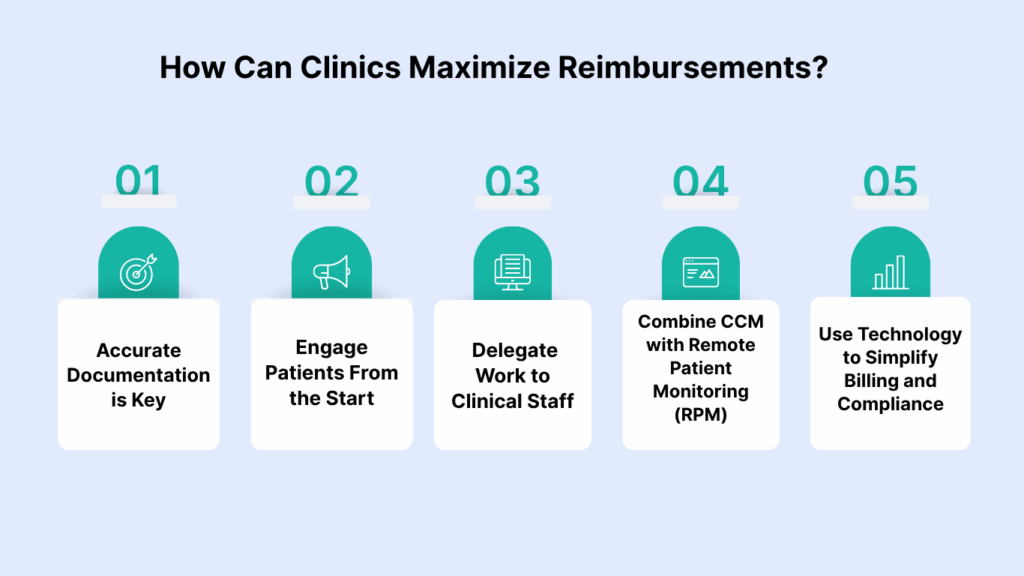
1. Accurate documentation is key
Medicare requires detailed records of time spent on each patient. Every phone call, medication check, or care plan update should be tracked. Without clear documentation, claims may be denied. Using software or platforms that automatically log time can reduce errors and protect revenue.
2. Engage patients from the start
Patients must give consent to enroll in CCM, and they should understand the benefits clearly. When patients know that CCM helps prevent complications and hospital visits, they are more likely to stay enrolled long term.
3. Delegate work to clinical staff
CPT 99490 and 99439 allow clinical staff time under physician supervision to be billed. By training your nurses or medical assistants to handle care coordination tasks, providers can save time while still being reimbursed.
4. Combine CCM with remote patient monitoring
CCM and RPM can be billed together for eligible patients. For example:
- CCM (99490): ~$62 per month
- RPM (99454 + 99457): ~$110 per month
Together, that’s $170+ per patient per month. For 50 patients, that equals $8,500 monthly — a powerful revenue stream that also improves patient care.
5. Use technology to simplify billing and compliance
Many platforms help clinics track patient data, document time, and generate reports that meet Medicare’s billing rules. Automating these steps reduces staff burden and ensures you don’t miss eligible reimbursements.
How Much Does Medicare Pay for Chronic Care Management?
The Bigger Picture with RPM
While CCM on its own pays between $62 and $147+ per patient, per month, clinics can unlock even more value by combining it with Remote Patient Monitoring (RPM). These two programs are designed to work hand in hand.
- CCM covers care planning, medication reviews, and coordination between providers.
- RPM tracks real-time patient data, like blood pressure or glucose levels, from home devices.
When billed together, providers can generate $170+ per patient each month. For example:
- CCM (99490): ~$62
- RPM (99454 + 99457): ~$110
- Total: ~$172 per patient/month
If a clinic enrolls 50 patients, that’s over $8,500 per month while giving patients a higher level of support.
The benefits for patients are just as important as the financial side. With both CCM and RPM in place, patients receive more consistent follow-ups, early detection of worsening symptoms, and fewer hospital visits. They also feel more connected to their care team, knowing someone is monitoring their progress even when they’re at home.
By combining CCM and RPM, providers not only increase revenue but also build stronger, more trusting relationships with patients who need ongoing support for chronic conditions.
Final Thoughts
Medicare’s Chronic Care Management program is a way for providers to give patients better long-term care while creating steady revenue for their clinic.
On its own, CCM brings in $62–$147+ per patient each month, and when combined with Remote Patient Monitoring, the total can exceed $170 per patient monthly. For even a small panel of patients, that adds up to meaningful income and measurable improvements in patient health.
The key is managing it the right way. Accurate documentation, consistent patient engagement, and the smart use of technology all make the difference in running a successful program.
Frequently Asked Questions (FAQs)
1. What conditions qualify for Chronic Care Management?
Medicare requires that patients have two or more chronic conditions expected to last at least 12 months or until death. The conditions must also place the patient at risk of decline or death if not managed properly. Examples include: diabetes, hypertension, heart disease, COPD, arthritis, depression, Alzheimer’s disease, and asthma.
2. Does Medicaid pay for Chronic Care Management?
Medicaid coverage for CCM is not the same in every state. Some states reimburse providers for care coordination similar to Medicare’s program, while others do not. To confirm, providers need to check state-specific Medicaid guidelines or reach out to their Medicaid managed care plans.
3. How is Chronic Care Management billed?
Chronic Care Management is billed monthly using CPT codes. The most common ones are:
- 99490: ~$62 for at least 20 minutes of clinical staff time under physician supervision.
- 99439: ~$47 for each additional 20 minutes.
- 99491: ~$85 for 30 minutes of provider (physician/NP/PA) time.
- 99437: ~$60 for each additional 30 minutes.
Providers must document time spent and have a care plan in place to bill successfully.
4. What is Chronic Care Management?
Chronic Care Management (CCM) is a Medicare program that pays providers for coordinating care outside of office visits for patients with multiple chronic conditions. This includes medication reviews, follow-up phone calls, coordinating with specialists, and adjusting care plans. The goal is to improve outcomes, reduce hospital visits, and support patients between appointments.
5. Where can I find a Chronic Care Management template PDF?
Medicare does not publish a universal template, but many EHR systems and healthcare compliance platforms provide CCM care plan templates. These templates usually include patient details, a list of chronic conditions, medications, treatment goals, and scheduled follow-ups. Providers must ensure any template they use meets CMS documentation requirements.
6. What is the Medicare chronic conditions list?
Medicare does not have a single official list, but examples of qualifying conditions include:
- Hypertension (high blood pressure)
- Diabetes
- Chronic obstructive pulmonary disease (COPD)
- Heart disease (CHF, coronary artery disease)
- Arthritis
- Cancer (active treatment)
- Alzheimer’s disease and other dementias
Any condition that is chronic, expected to last at least 12 months, and poses a risk if unmanaged may qualify.
7. Can you give examples of Chronic Care Management?
Yes. Examples of CCM include:
- A nurse calling a patient with diabetes to review medications and recent blood sugar readings
- A care coordinator helping a heart disease patient adjust medications and schedule lab work.
- Updating a care plan for a COPD patient after an ER visit.
- Coordinating between a primary care doctor and a specialist for a patient with multiple conditions.
8. What are the CPT codes for Chronic Care Management?
The main CPT codes are:
- 99490 – Non-complex CCM, 20 minutes of staff time.
- 99439 – Add-on code for each extra 20 minutes.
- 99491 – 30 minutes of provider time (physician/NP/PA).
- 99437 – Add-on code for each extra 30 minutes of provider time.
These codes allow providers to bill based on time and complexity of care.
9. What are Medicare’s guidelines for Chronic Care Management?
According to CMS, providers must:
- Obtain patient consent before enrolling in CCM
- Create and maintain a comprehensive care plan.
- Track and document time spent on non-face-to-face care coordination.
- Offer 24/7 access for urgent needs.
Bill only once per patient per month, using add-on codes if more time is spent.