Remote Patient Monitoring (RPM) helps doctors check a patient’s health from home. Patients use simple devices like blood pressure cuffs or glucose meters. These devices send health readings to their doctor through a secure system.
Doctors can see the results in real time, notice any changes, and help before things get worse. It’s an easy way to stay connected and stay healthy without going to the clinic.
This blog will explain how remote patient monitoring works, step by step, in the simplest way possible.
How Does Remote Patient Monitoring Work?
To understand how RPM works, it is important to know the main parts that make it run. Each part plays a simple but important role in keeping care smooth and connected. Here are the main components of an RPM program:
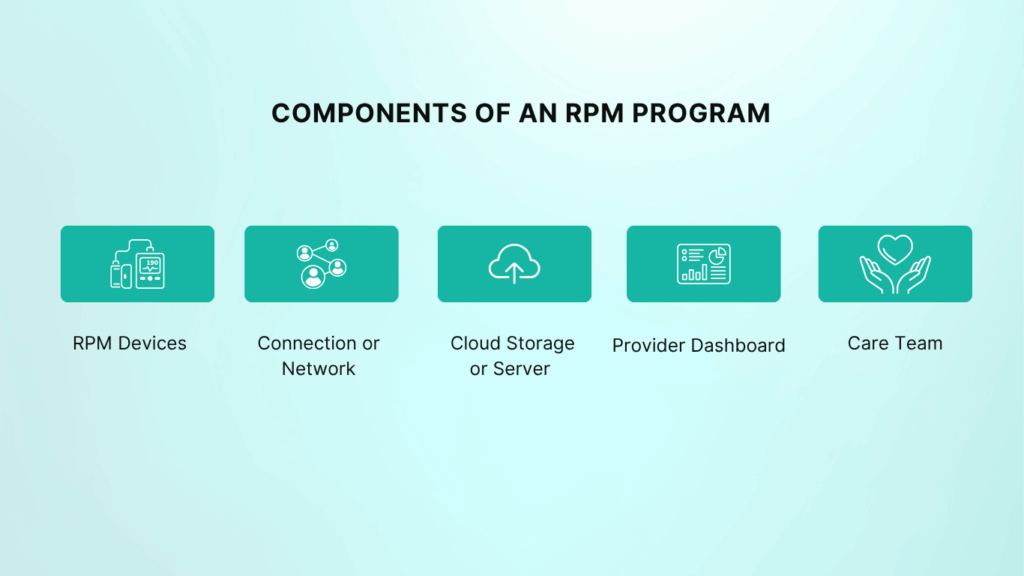
1. RPM Devices
These are the tools patients use at home. They can be blood pressure cuffs, glucose meters, pulse oximeters, or weight scales. Most of these devices work automatically, you just take your reading, and the device sends the result.
2. Connection or Network
Devices send the data through a secure connection. Some use Wi-Fi, while others like CandiHealth use built-in cellular networks (no internet setup needed). This means even patients in rural areas can stay connected.
3. Cloud Storage or Server
Once the reading is taken, the data travels to a secure cloud system. This is where it’s stored safely so doctors and nurses can access it anytime.
4. Provider Dashboard
Doctors and care teams log in to a dashboard to see each patient’s daily readings. They can spot trends, track improvements, or get alerts if something looks off.
5. Care Team
Behind the system, there’s a team (nurses, doctors, and support staff) who review the data, contact patients when needed, and help with treatment changes.
Together, these parts make RPM simple yet powerful. The patient only has to use the device, and everything else happens automatically.
Step-by-Step: How Remote Patient Monitoring Works
Here is the step by step process explaining how remote patient monitoring works in real life.
- Doctor enrolls patients into RPM program
- The doctor teaches patients how to use RPM devices.
- The patient takes reading using the medical device.
- The device automatically transmits data to the provider dashboard.
- The doctor or the care team reviews the data and follows up.
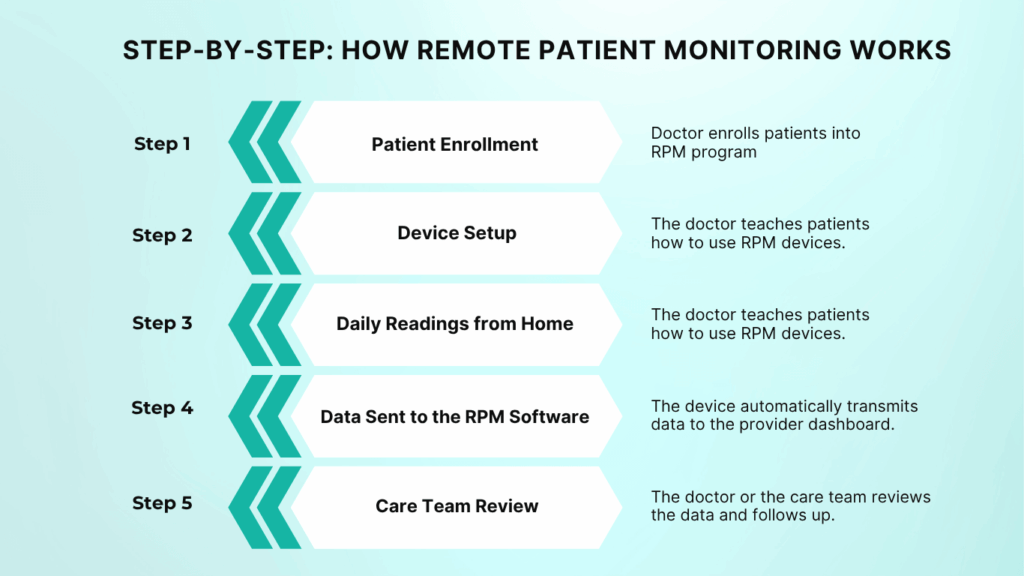
Here is the detailed description of each step of how the remote patient monitoring works.
1. Patient Enrollment
The process starts when a doctor decides that a patient could benefit from RPM. This is often someone with high blood pressure, diabetes, or another long-term condition. The clinic registers the patient and gives them an RPM device, like a cellular blood pressure monitor.
2. Device Setup
The patient is shown how to use the device. Most devices are already connected, so there’s no app or Wi-Fi needed. The patient just turns it on and takes a reading.
3. Daily Readings from Home
Each day, the patient takes their readings at home. The device automatically sends the results to the clinic’s system. There’s no paperwork or extra steps needed.
4. Data Sent to the RPM Software
The device sends the data securely to a cloud platform. This system keeps the data safe and private, following healthcare privacy laws like HIPAA.
5. Care Team Review
Doctors or nurses check the data on their dashboard. They can see every patient’s latest readings, spot trends, and get alerts if something looks unusual — like a sudden rise in blood pressure.
6. Doctor Follows Up
If there’s a problem, the care team calls the patient. The doctor may suggest a medicine change, schedule a visit, or simply give advice.
7. Ongoing Monitoring and Billing
Every month, the clinic tracks how much time was spent reviewing data and contacting patients. They use Medicare codes (99453, 99454, 99457, and 99458) to bill for the service.
That’s it — a simple, daily loop of taking readings, sending data, and staying connected.
With RPM, patients stay cared for between visits, and doctors get the full picture of their health without waiting for the next appointment.
Example: How RPM Works for a Hypertension Patient
Let’s look at how Remote Patient Monitoring works for someone with high blood pressure.
Meet Jones, a 58-year-old patient who has been struggling to keep his blood pressure under control. His doctor enrolls him in an RPM program and gives him a cellular blood pressure monitor to use at home.
1. Daily Use
Every morning, Jones wraps the cuff around his arm and presses a single button. Within a few seconds, his reading appears on the device screen, and is automatically sent to his doctor through a secure connection.
2. Automatic Data Sharing
Jones doesn’t need to write anything down or open any app. His readings reach the clinic dashboard in real time, where the nurse can see if his numbers are stable or rising.
3. Continuous Monitoring
For a few days, everything looks fine. But one morning, his blood pressure was higher than usual. The system instantly flags it on the doctor’s dashboard.
4. Quick Follow-Up
The nurse calls Jones the same day to check if he’s feeling okay and whether he missed his medicine. After a short discussion, the doctor adjusts his medication and asks him to continue daily readings.
5. Better Control Over Time
Over the next few weeks, Jones’ numbers improved. He doesn’t have to visit the clinic every week, and his doctor can track his progress safely from a distance.
This example shows how RPM improves patient outcomes. Patients stay in control of their health, and doctors can act early, often preventing emergency visits. It’s an easy way to keep blood pressure and peace of mind steady.
Challenges and Best Practices for Using RPM
Remote Patient Monitoring is powerful, but like any healthcare system, it works best when used the right way. Here are some common challenges and how clinics can manage them smoothly:
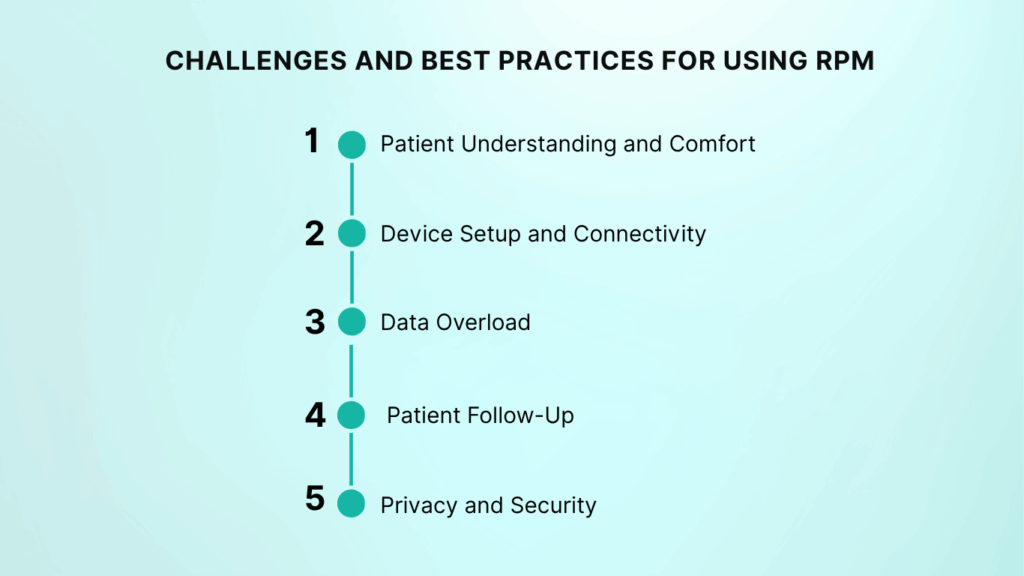
1. Patient Understanding and Comfort
Some patients, especially older adults, may feel nervous using new devices. The best approach is to keep things simple. Provide clear instructions and quick training when they receive the device. A short demo or printed guide can make a big difference.
2. Device Setup and Connectivity
Wi-Fi–based devices can be tricky for patients who live in rural areas or have limited internet access. Choosing cellular-enabled devices solves this problem because they send readings automatically without needing Wi-Fi or smartphone apps.
3. Data Overload
When many patients send daily readings, the care team can receive a lot of data. The solution is to use an RPM platform that highlights abnormal readings or trends, so staff can focus only on what matters most.
4. Patient Follow-Up
RPM only works when there’s communication. Clinics should create a clear plan for who reviews data each day and how alerts are handled. For example, nurses can call patients if their readings are high before the doctor reviews them.
5. Privacy and Security
Protecting patient information is critical. Every RPM platform should follow HIPAA rules and use strong encryption to keep data safe. Clinics should also remind patients not to share device details with others.
Best Practices for Successful RPM Program:
- Choose devices that are easy to use and ready to connect.
- Give patients short, friendly training sessions.
- Use dashboards that highlight alerts automatically.
- Set up a daily routine for reviewing readings.
- Keep all communication secure and respectful.
By following these best practices, clinics can get the most out of RPM — fewer errors, better patient trust, and smoother workflows.
The Future of Remote Patient Monitoring
Remote Patient Monitoring is growing fast, and its future looks even more promising. As technology improves, RPM will become an even bigger part of everyday healthcare.
1. Smarter Technology
New RPM systems are being built with artificial intelligence (AI). These tools can study data from many patients, notice early warning signs, and send automatic alerts to doctors before problems get serious. AI can even predict who might need extra care soon.
2. Expansion Beyond Chronic Care
Right now, RPM is mostly used for conditions like high blood pressure, diabetes, and heart disease. But in the future, it will expand to areas like mental health, post-surgery recovery, and elderly care. This means more people will benefit from remote monitoring.
3. Easier Use for Patients
Future devices will be smaller, faster, and easier to use — some may work through simple patches or smartwatches. The goal is to make monitoring feel natural, not like a chore.
4. Better Integration with Health Systems
Hospitals and clinics will link RPM data directly with their electronic health records (EHR). This will give doctors a complete picture of a patient’s health — both in and out of the clinic.
5. Support from Medicare and Insurance
With proven results in reducing hospital readmissions and improving outcomes, more healthcare programs and insurers are likely to expand RPM coverage. This will help more clinics adopt it without financial barriers.
In short, the future of RPM is about smarter care and stronger connection. It will keep patients safer, help doctors make faster decisions, and bring healthcare even closer to home.
Final Thoughts
Remote Patient Monitoring works by connecting patients and doctors through simple, smart devices. Each reading taken at home helps doctors track progress, spot risks early, and adjust care before small issues turn serious.
It’s an easy, reliable way to keep patients healthier and reduce hospital visits — all while giving doctors the full picture between appointments.
Want to start Remote Patient Monitoring at your clinic?
See how CandiHealth makes RPM simple with pre-configured cellular devices, real-time dashboards, and a flat $10 per-patient model.
Frequently Asked Questions (FAQs)
1. How does a remote monitoring system work?
A remote monitoring system works by collecting a patient’s health data through RPM medical devices at home. These devices send readings to a secure digital platform. The doctor or nurse reviews the data in real time and reaches out if something looks unusual. This helps detect problems early and keeps care continuous between clinic visits.
2. Does remote patient monitoring work?
Yes, remote patient monitoring (RPM) works very well for patients with chronic conditions like high blood pressure or diabetes. It gives doctors regular updates without needing in-person visits, helping them adjust treatment plans early. Studies show RPM programs reduce hospital visits, improve blood pressure control, and increase patient satisfaction.
3. How does a remote medical device work?
A remote medical device measures specific health metrics and sends that data to the care team. Devices can use Wi-Fi or built-in cellular networks to share readings automatically. Doctors receive this information through a secure dashboard and can act quickly if they notice any changes.
4. What are remote patient monitoring devices?
Remote patient monitoring devices are tools that collect health readings at home. These include:
- Blood pressure monitors
- Glucometers
- Pulse oximeters
- Weight scales
- Smart thermometers
They gather patient data automatically and send it to healthcare professionals for review, making it easier to manage long-term conditions without constant clinic visits.
5. What is the most popular remote patient monitoring program?
There are several trusted RPM programs in the U.S., but CandiHealth stands out for its simplicity and cost-effectiveness. CandiHealth offers pre-configured cellular RPM devices, so patients don’t need Wi-Fi or apps. Clinics get real-time dashboards, automated alerts, and an easy billing process, all for a flat $10 per patient with no extra fees.
It’s a practical solution for clinics looking to start or scale their RPM program without technical hurdles or hidden costs.
6. What conditions benefit from RPM?
Remote Patient Monitoring helps manage a wide range of chronic and long-term conditions, including:
- Hypertension (high blood pressure)
- Diabetes
- Heart disease
- COPD and respiratory illnesses
- Obesity and weight management
- Post-surgical recovery
Patients with these conditions benefit from daily monitoring, fewer emergency visits, and a stronger connection with their healthcare team.