In July 2025, the Centers for Medicare & Medicaid Services (CMS) released the 2026 Physician Fee Schedule (PFS) Proposed Rule. One of the key highlights is the introduction of a new CPT code 99XX5 for Remote Patient Monitoring (RPM) treatment management.
Currently, providers can only bill CPT 99457 when they spend 20 minutes or more each month managing a patient’s RPM data. This means if a provider spends 10 or 15 minutes reviewing readings (like blood pressure or glucose) and making a quick phone call, they cannot bill for that time. Those shorter interactions are not reimbursed.
CPT 99XX5 is designed to close that gap. If finalized, it would allow providers to bill for 10–20 minutes of RPM care time each month, as long as there’s at least one real-time, interactive patient communication. This guide explains
- What CPT 99XX5 covers
- How it compares to existing RPM codes,
- Who can bill CPT 99XX5
and how practices can prepare now for its potential rollout on January 1, 2026.
Table of Contents
What Is CPT Code 99XX5? Key Details Explained
Here’s what healthcare providers in USA need to know about CPT 99XX5 based on the CMS 2026 PFS Proposed Rule and the AMA CPT Panel:
1. CPT Code 99XX5 Status
CPT 99XX5 is a proposed code in the 2026 Medicare Physician Fee Schedule. It will not become active until the Final Rule is published (Nov 2025) and, if finalized, will take effect January 1, 2026【Federal Register – CY 2026 PFS Proposed Rule】.
2. 99XX5 Description (What does it cover?)
Remote physiologic monitoring treatment management services, 10–19 minutes of clinical staff/physician time per calendar month, with at least one real-time interactive communication with the patient or caregiver【AUA Policy Summary of 2026 PFS】.
3. 99XX5 Time Threshold
This code is Billable for 10–20 minutes of RPM management time in a calendar month.
- If <10 minutes, not billable.
- If ≥20 minutes, use CPT 99457 instead.
The code requires at least one live, real-time interaction with the patient or caregiver (phone or video). 【CMS Proposed Rule】.
4. 99XX5 Billing Frequency
This code can be billed once per patient per calendar month. Moreover CPT 99XX5 and CPT 99457 cannot both be billed in the same month for the same patient. You must choose one based on total time. However, CPT 99XX5 can be combined with CPT 99458 (add-on code) if total time exceeds 20 minutes.
5. 99XX5 Reimbursement Rate
CMS proposes reimbursement rate at about half of CPT 99457. Estimated national average Medicare rate: ~$23.73, compared to ~$47.87 for 99457【Federal Register PFS 2026】.
6. 99XX5 Documentation Requirements
Providers must document:
- Total minutes spent on RPM management (≥10, <20).
- Details of clinical actions (review of data, communication, medication changes).
- Date & mode of real-time interaction with patient/caregiver.
Who Can Bill CPT 99XX5? (Eligible Providers)
The claim for CPT 99XX5 must be submitted by a provider who has a National Provider Identifier (NPI) and is authorized to bill Medicare for RPM services. Eligible practitioners include:
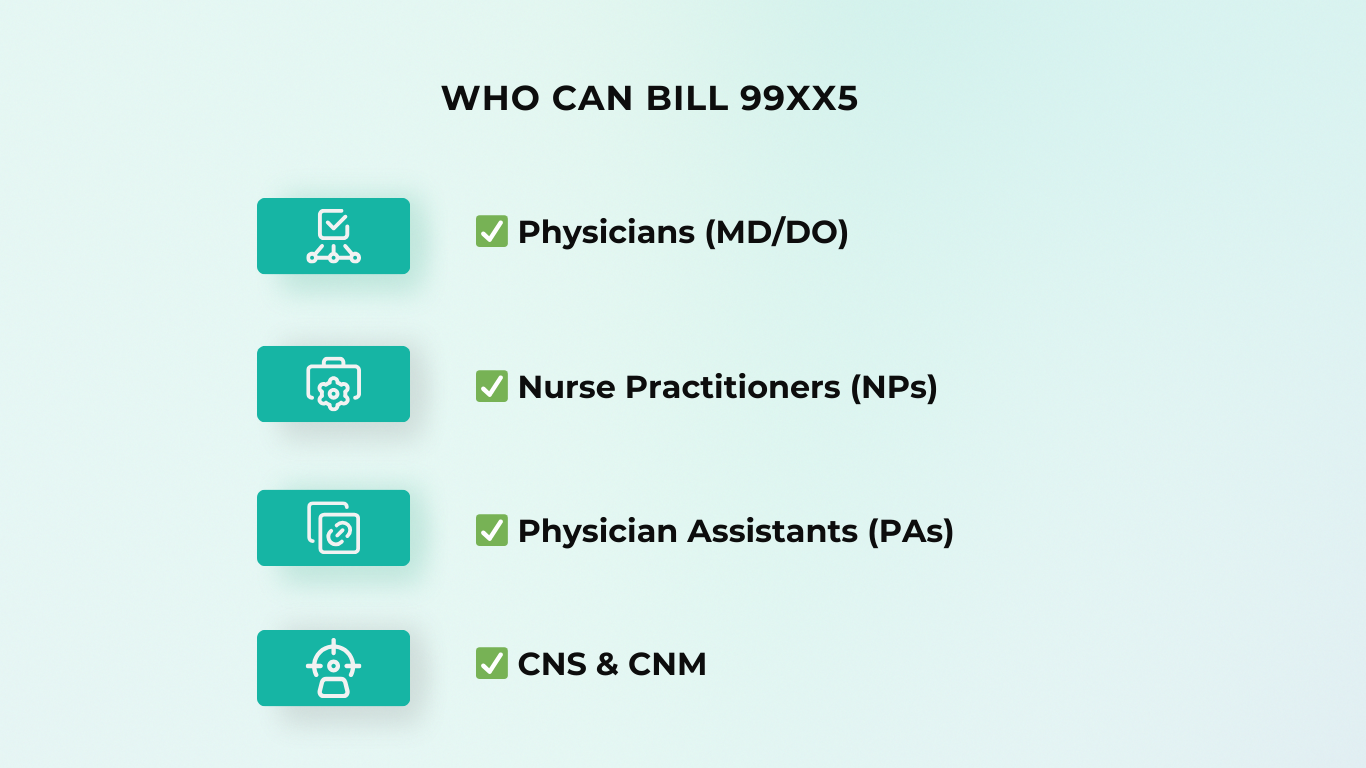
- Physicians (MD/DO)
- Nurse Practitioners (NPs)
- Physician Assistants (PAs)
- Clinical Nurse Specialist
- Certified Nurse Midwives
Role of Clinical Staff
Clinical staff time counts toward the 10–20 minutes, as long as it is provided under the general supervision of a billing provider. This means registered nurses (RNs), licensed practical nurses (LPNs), or other care team members can perform RPM activities, but the supervising provider bills the service.
Why CMS Introduced CPT 99XX5
When CMS first created RPM billing codes (like CPT 99457 in 2019), the rule required providers to spend at least 20 minutes per month on patient management before they could bill【CMS 2019 Final Rule – RPM Codes】. However, many RPM interactions are shorter than 20 minutes but still clinically important. For example, a provider might:
- Spend 12 minutes reviewing a week of blood glucose readings.
- Call a patient briefly to adjust their hypertension medication.
- Perform a 15-minute post-discharge check-in to ensure a patient is stable.
Under today’s rules, none of these encounters are billable, even though they provide real medical value.
Professional groups like the AMA CPT Editorial Panel and specialty societies argued that this 20-minute minimum created a reimbursement gap. It discouraged providers from engaging in short but meaningful RPM check-ins, because the work went unpaid【AMA CPT Editorial Panel Summary】.In response, the AMA approved CPT 99XX5 in 2024, and CMS included it in the 2026 PFS Proposed Rule.
CMS proposes to value 99XX5 at about 50% of CPT 99457’s payment. This means if CPT 99457 reimburses ~$50, CPT 99XX5 would pay around $25. The goal is to reward shorter RPM interactions without replacing the existing 20-minute code.
Benefits of CPT 99XX5 for RPM Programs
The proposed CPT 99XX5 adds much-needed flexibility to Remote Patient Monitoring (RPM) billing. Here are some of the benefits of CPT 99XX5 for RPM programs:
1. Greater Flexibility for Healthcare Providers
With CPT 99XX5, practices in the USA no longer lose reimbursement if their monthly RPM time falls just under 20 minutes. This encourages providers to engage patients more often, without worrying about “wasting” time that doesn’t reach the billing threshold.
2. Better Patient Care
Short check-ins are often the difference between stability and complications. For example, a 15-minute follow-up call after a medication change can catch side effects early. By making these billable, CMS is reinforcing the value of proactive care rather than reactive care.
3. Expanding Access to RPM
Many patients, especially those with chronic conditions, don’t always need 20+ minutes of monthly management. CPT 99XX5 allows providers to still engage those patients meaningfully, while making the service financially sustainable.
This could expand RPM to smaller clinics and rural providers, where quick, frequent touchpoints are more common【CMS Proposed Rule】.
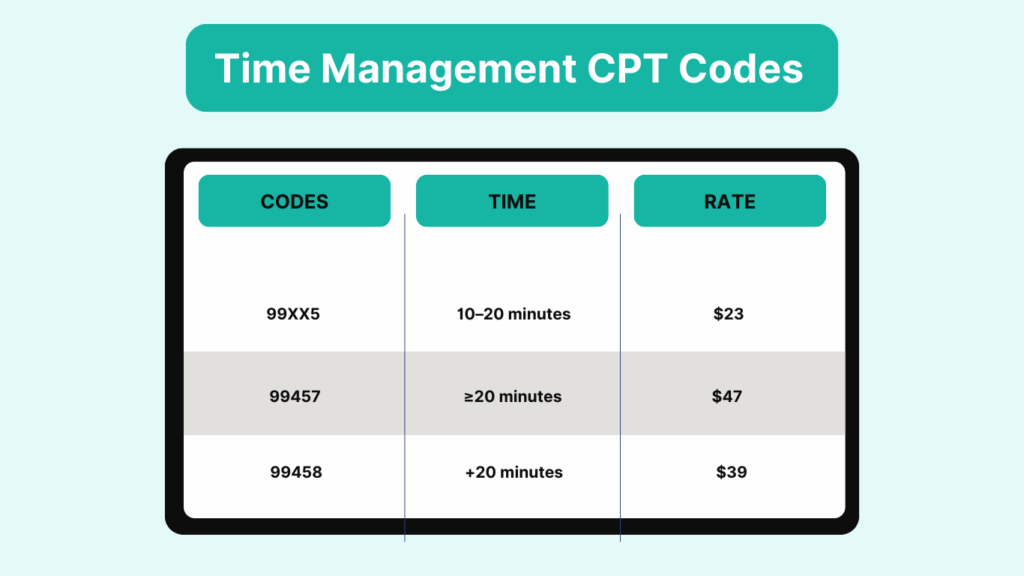
CPT 99XX5 vs. 99457 vs. 99458: Key Differences
The RPM time-based codes now fall into tiers. Here is a brief overview of the key differences between RPM time management codes. It is important to understand how they work together for accurate billing and compliance.
Code Breakdown
| CPT Code | Time Threshold | Requirements | Remboursement rate (2026 est.) | When to Use |
| 99XX5 (Proposed) | 10–20 minutes | ≥1 live, real-time patient/caregiver interaction | ~$25.73 | When total monthly RPM time is 10–20 minutes. |
| 99457 | ≥20 minutes (first 20) | ≥1 live, real-time interaction | ~$49.46 | When monthly RPM time reaches 20 minutes or more |
| 99458 | Each additional 20 minutes | Must follow 99XX5 or 99457 | ~$39.77 | When total RPM time exceeds the base code (e.g., 30–40 minutes, bill add-on) |
Final Thoughts
The proposed CPT 99XX5 is more than just a new billing code — it’s a recognition that shorter RPM interactions (10–19 minutes) still deliver meaningful care. By filling the reimbursement gap left by CPT 99457’s 20-minute minimum, it ensures providers are paid fairly for work they are already doing.
If finalized, CPT 99XX5 will take effect on January 1, 2026. Practices that prepare now by training staff, updating workflows, and tracking short RPM sessions will be ready to capture this new revenue stream from day one.
Frequently Asked Questions About CPT 99XX5
1. Is CPT 99XX5 finalized?
No. CPT 99XX5 is still proposed in the 2026 Medicare Physician Fee Schedule (PFS) Proposed Rule. The final rule will be published in November 2025, and if approved, the code will be effective January 1, 2026.
2. How much time does CPT 99XX5 cover?
CPT 99XX5 covers 10–20 minutes of RPM treatment management services in a calendar month. If providers spend 20 minutes or more, they should use CPT 99457 instead.
3. Can I bill CPT 99XX5 and CPT 99457 in the same month?
No. They are mutually exclusive. Providers must choose one code each month based on total RPM time:
- 10–20 minutes → CPT 99XX5
- 20+ minutes → CPT 99457
5. Who can bill CPT 99XX5?
Physicians and advanced practice providers (NPs, PAs, CNS, CNM) may bill CPT 99XX5. Clinical staff time counts if performed under general supervision of a billing provider.