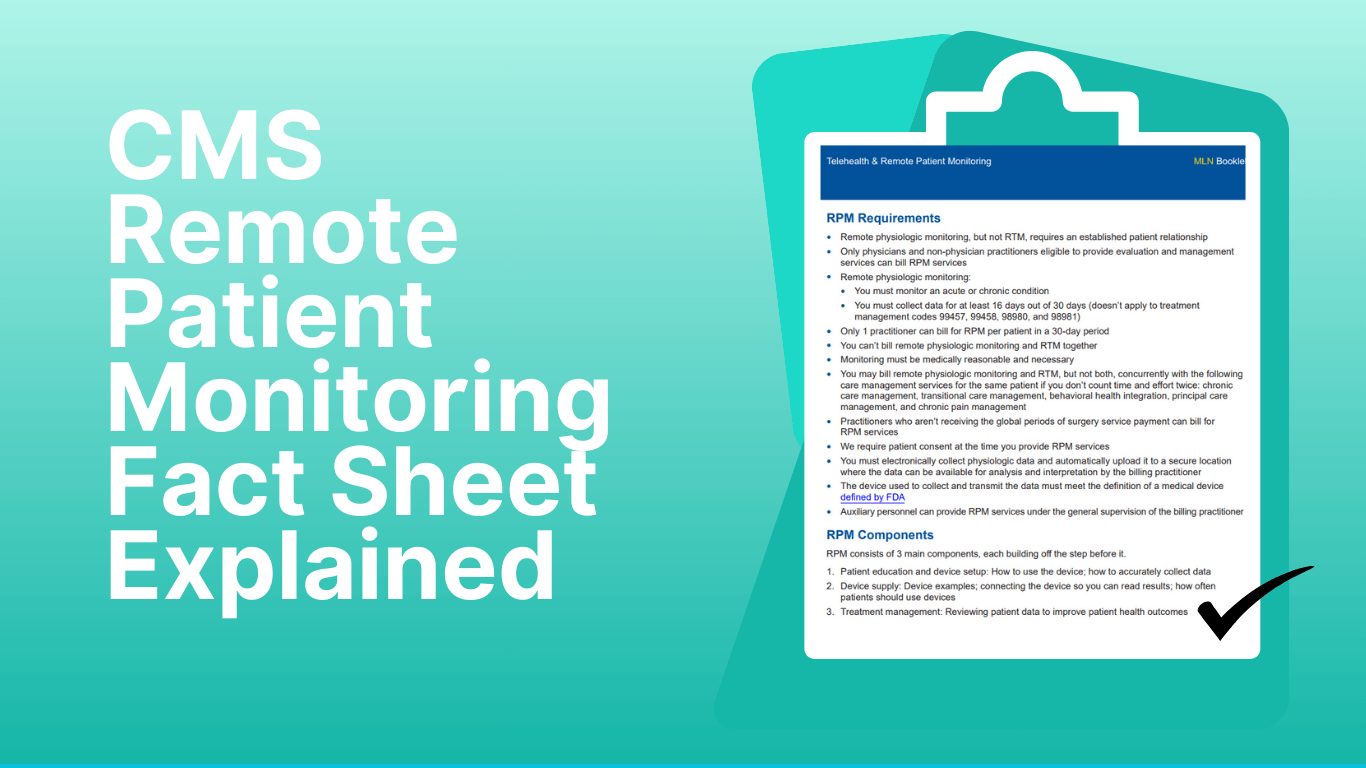
The Centers for Medicare & Medicaid Services (CMS) regularly publishes fact sheets and Medicare Learning Network (MLN) booklets to guide providers. The latest CMS Remote patient monitoring facts sheet, MLN901705 (Telehealth & Remote Patient Monitoring, April 2025), gives clear instructions on how RPM should be set up, billed, and documented under Medicare rules.
But, why does this matter? Because CMS and the Office of Inspector General (OIG) have already flagged problems: too many RPM claims are missing key elements, such as proper documentation of interactive patient communication . That means practices that treat RPM casually risk audits, clawbacks, and denied claims.
At the same time, the opportunity is huge. RPM allows providers to track patients with chronic and acute conditions in real time, intervene earlier, and reduce hospital visits. When used correctly, and billed according to CMS rules, it can become both a revenue stream and a patient engagement tool.
What Is the CMS RPM Fact Sheet?
The CMS Remote Patient Monitoring Fact Sheet is an official resource published through the Medicare Learning Network (MLN901705, April 2025). Its purpose is to help providers “use and bill correctly” for RPM services under Medicare.
Here’s what the fact sheet includes:
- What RPM is (and isn’t)
- Who can bill and when
- Device and data requirements
- The 16-day rule
- Common billing cpt codes
- Documentation requirements
- Common billing mistakes
- Clinic workflow
Let’s break down each component of the CMS Remote Patient Monitoring Fact Sheet in detail..
1. How CMS Defines Remote Patient Monitoring
According to CMS, Remote Patient Monitoring (RPM) means using a medical device that meets FDA standards to collect and transmit patient health data digitally. The data must be sent automatically to the provider for review and follow-up care. Examples of data CMS accepts:
- Blood pressure readings
- Blood glucose levels
- Weight measurements
- Pulse oximetry (oxygen saturation)
RPM vs. RTM. What’s the difference?
CMS makes a distinction between Remote Physiologic Monitoring (RPM) and Remote Therapeutic Monitoring (RTM). RPM deals with physiologic data (like a blood pressure reading). RTM covers therapy-related data, often reported by the patient (like medication use or pain scores).
Three Core Components of RPM Defined by CMS
CMS makes it clear that to bill Medicare correctly, you must deliver three core components. Each one is tied to specific CPT codes.
1. Setup and Patient Education
Covers the initial setup of the device and teaches the patient how to use it. Example: Training a patient to take daily blood pressure readings and showing them how results are sent to the clinic automatically.
2. Device Supply and Data Transmission
This component covers providing the device and receiving data. CMS requires the device to be FDA-cleared and transmit data automatically.
3. Treatment and Management
This component covers the time spent by doctor and staff in reviewing the patient data to improve health outcomes.
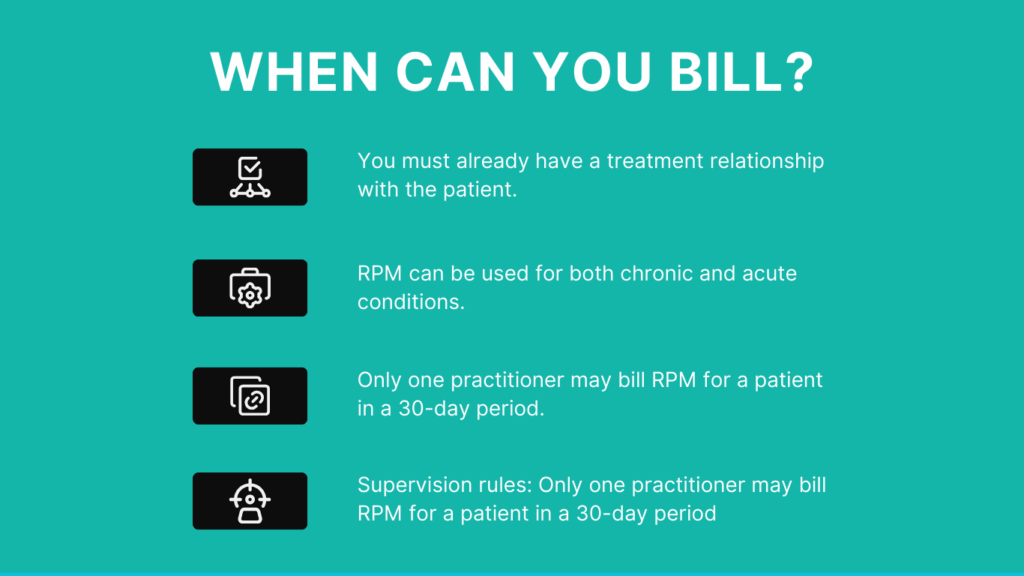
2. Who Can Bill RPM and When
Not every clinic staff member can submit RPM claims. CMS sets clear rules about who is eligible to bill and under what conditions.
Who can bill RPM?
1. Physicians (MD, DO) and qualified non-physician practitioners (such as nurse practitioners and certain clinical nurse specialists) can bill for RPM.
2. Auxiliary staff (like medical assistants or nurses) can perform many of the day-to-day tasks, such as device setup or patient follow-ups, but they must work under the general supervision of the billing provider.
Example:
A nurse sets up the device for the patient, but only the supervising doctor bills for the service at the end of the 30-day cycle.
When can you bill?
- You must already have a treatment relationship with the patient.
- RPM can be used for both chronic and acute conditions.
- Only one practitioner may bill RPM for a patient in a 30-day period.
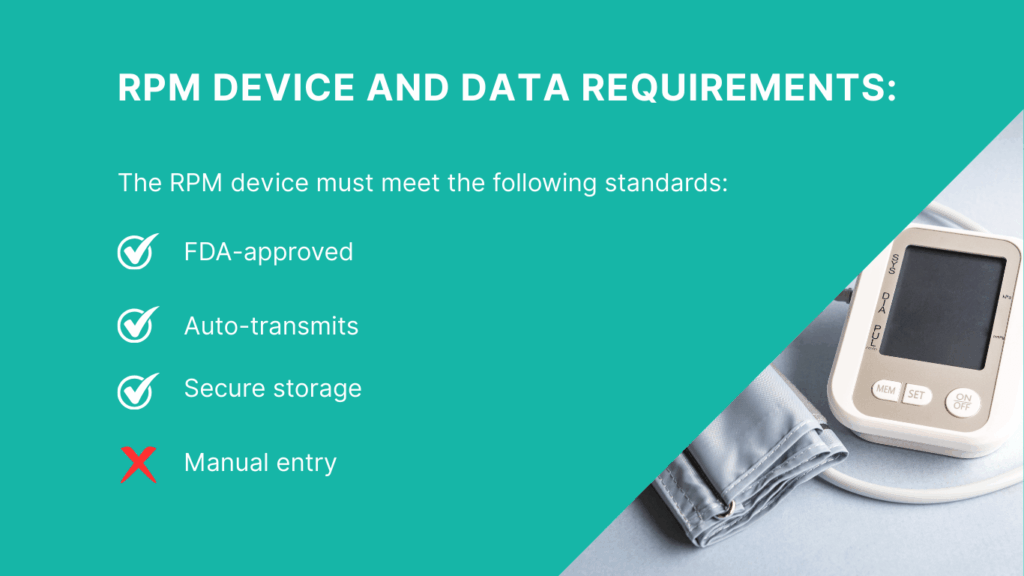
3. Device & Data Requirements by CMS
To be billable, the device must meet remote patient monitoring billing guidelines cms
1. It must be an FDA medical device.
That means it has been cleared by the FDA to measure vital signs or physiologic data. A fitness tracker or smartwatch, for example, usually won’t count unless it is FDA-approved for medical use
2. It must automatically transmit data.
The device must send readings directly to a secure system. Manual entry does not meet CMS requirements.
3. It must store and send data securely.
The information should flow into a system where the provider can review, analyze, and document it. Privacy and HIPAA compliance are part of this rule.
Note: When devices meet these conditions, teams spend less time chasing data and more time making care decisions. That’s why systems like CandiHealth use pre-configured cellular monitors that send readings automatically. The data arrives in the clinic dashboard without Wi-Fi or apps, keeping the process smooth for both patients and staff.
4. The 16-Day Rule Requirement by CMS
One of the most important remote patient monitoring medicare billing guidelines is the 16-day rule. For code 99454 (device supply and data transmission), you must have at least 16 days of patient data in a 30-day period. Anything less, and that code cannot be billed.
Where it doesn’t apply: The 16-day requirement is only for device supply. It does not apply to treatment management codes like 99457 or 99458. These can still be billed as long as the provider meets the required time spent with the patient.
Why it matters: Missing this rule is one of the most common reasons claims are denied. Tracking day counts carefully helps prevent problems at audit time.
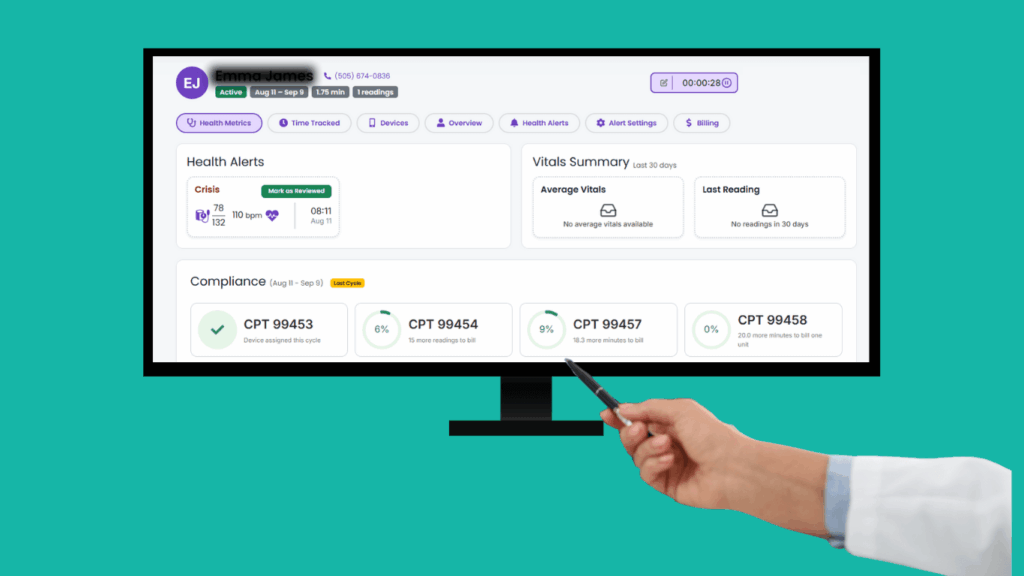
5. Common RPM Billing Codes
CMS uses a set of CPT codes for Remote Patient Monitoring. Each code applies to a different part of the process:
| CPT Code | What It Covers | Key Requirement |
| 99453 | Initial setup and patient education | Billed once per episode of care |
| 99454 | Device supply and data transmission | At least 16 days of data in a 30-day period |
| 99457 | First 20 minutes of treatment management | Interactive communication with the patient; audio-only allowed |
| 99458 | Additional 20 minutes of treatment management | Used only as an add-on to 99457; audio-only allowed |
| 99091 | Review and interpretation of physiologic data | Requires 30 minutes of provider time per month |
For many clinics, the challenge is making sure the right code matches the right service. Having a system that logs setup, device activity, and interaction time helps reduce errors. In CandiHealth, these logs are tracked automatically, so staff can confirm which codes apply before submitting claims.
6. Common Mistakes to Avoid When Billing RPM
Even experienced teams run into issues with RPM billing. The CMS fact sheet highlights common mistakes that often lead to denials:
| Common Mistakes | Why It’s a Problem |
| Counting manual entries as data | CMS only accepts data automatically transmitted from an FDA-approved device. |
| Missing consent | Without documented patient consent, RPM services are not billable. |
| Double billing | Only one provider can bill RPM for a patient in a 30-day period. |
| Weak documentation of time | For 99457/99458, CMS requires proof of interactive time spent with the patient. |
| Incomplete programs | OIG has flagged cases where RPM was billed without all components (setup, supply, management). |
Avoiding these pitfalls saves time and reduces the risk of audits.
A Simple Clinic Workflow for RPM
Putting the fact sheet into practice can feel overwhelming at first. But if you break it down into steps, the process becomes much easier for both staff and patients. A straightforward workflow looks like this:
- First, identify patients who would benefit from RPM. Hypertension, heart disease, diabetes, and recovery from acute illnesses are common starting points. Once the patient is selected, confirm consent and document it in the record.
- Next, set up the device. The patient should be able to use it with minimal effort. Simplicity at this stage prevents drop-offs later. Readings then flow automatically into the clinic’s dashboard, where staff can review trends.
- Throughout the month, the care team tracks daily data and ensures the patient reaches the 16-day requirement. Providers also spend interactive time with the patient, checking on their progress and adjusting the care plan as needed.
- At the end of the cycle, the provider reviews the records, confirms that all requirements are met, and bills the correct CPT codes. When each step is consistent, RPM becomes a reliable part of routine care instead of an extra burden.
Platforms like CandiHealth support this flow by combining device setup, data collection, and time tracking in one place. This helps staff move through the process without worrying about missing a requirement.
Final Thoughts
The CMS Remote Patient Monitoring Fact Sheet gives clear guidance: use FDA-approved devices, track at least 16 days of data, document consent, and spend meaningful time with patients. When these steps are followed, RPM not only meets compliance requirements but also strengthens patient care.
For many clinics, the hardest part is keeping everything organized while still focusing on patients. That’s why simple tools matter. With CandiHealth, readings flow automatically from the device to the clinic dashboard, day counts are tracked in real time, and interaction time is logged. The result is fewer billing headaches and more attention on patient outcomes.
Frequently Asked Questions
What are the CMS billing guidelines for Remote Patient Monitoring?
CMS allows billing for RPM if you use FDA-approved devices, collect at least 16 days of data in 30 days (for code 99454), and document patient consent and provider interaction time. Each CPT code covers a different part of the service, such as setup, device supply, or treatment management.
What are the Medicare rules for RPM?
Medicare covers RPM for both chronic and acute conditions. The patient must be established with the provider, and only one practitioner can bill for RPM in a 30-day period. Auxiliary staff may help under general supervision.
What types of devices can be used for RPM?
Only FDA-defined medical devices qualify. They must capture physiologic data (like blood pressure or glucose) and automatically send readings electronically. Fitness trackers and manual logs don’t count.
Which CPT codes are used for RPM?
The most common codes are:
- 99453: Device setup and patient education (one-time).
- 99454: Device supply and transmission (≥16 days).
- 99457: First 20 minutes of patient management per month.
- 99458: Each additional 20 minutes.
- 99091: 30 minutes of provider time reviewing data.
What are the types of Remote Patient Monitoring?
There are two main categories:
- RPM: Focused on physiologic data like blood pressure, weight, or oxygen levels.
- RTM: Focused on therapy-related data like medication use or pain tracking, often self-reported by the patient.
What are the benefits of Remote Patient Monitoring?
RPM helps improve patient outcomes by catching changes early, reduces emergency visits, and supports chronic disease management. For clinics, it provides a new revenue stream while keeping patients engaged between visits.