Many healthcare providers in the U.S. hesitate to start a remote patient monitoring (RPM) program. They often ask questions like:
- Is it worth the effort?
- What if patients don’t take readings?
- Will Medicare deny our claims?
- How much revenue can we really make?
These are the concerns most healthcare providers in the U.S. share before taking the first step.
CandiHealth was built with those doubts in mind. With simple cellular blood pressure devices, an easy-to-use dashboard, and clear billing tools, it helps clinics launch RPM without extra burden on staff or risk to revenue.
In this guide, we’ll walk through how you can get started with CandiHealth — from checking eligibility to enrolling patients, handling billing, and making RPM part of daily care.
Key Features of CandiHealth RPM Platform
Below are the key features and components of CandiHealth’s remote BP monitoring program:
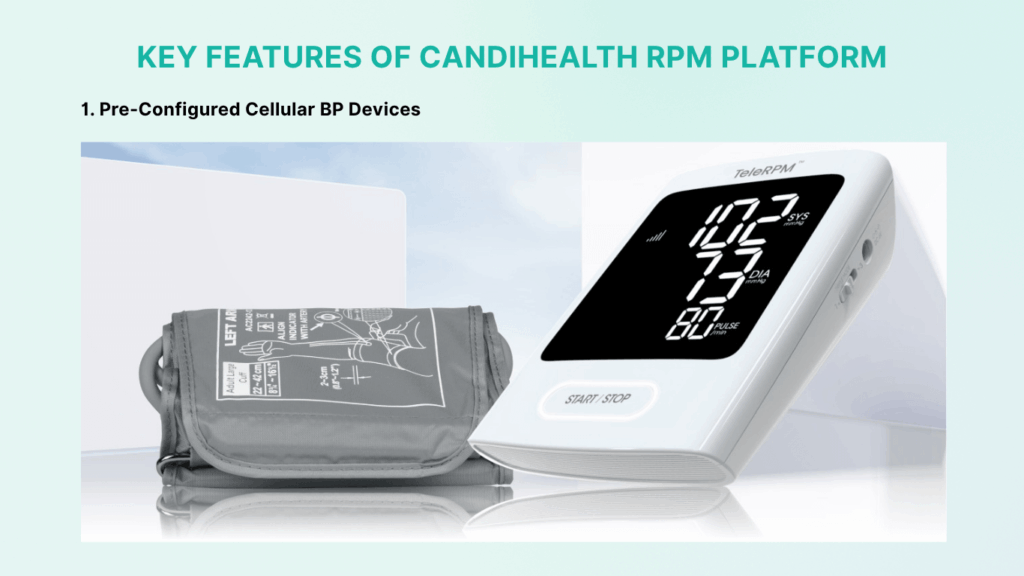
1. Pre-Configured Cellular BP Devices
CandiHealth provides FDA-cleared blood pressure cuffs that are ready to use. They come with built-in cellular service. Patients don’t need a smartphone, Bluetooth, or Wi-Fi. They just put on the cuff and press a button. The reading is sent automatically to the clinic dashboard. This makes onboarding quick and stress-free, especially for older patients or those who are not tech-savvy.
2. One-Hour Setup and Easy Onboarding
Clinics can add patients, assign devices, and go live in less than an hour. Devices can be shipped to the clinic or directly to patients. Staff can start monitoring the same day. No long training or complex setup is needed.
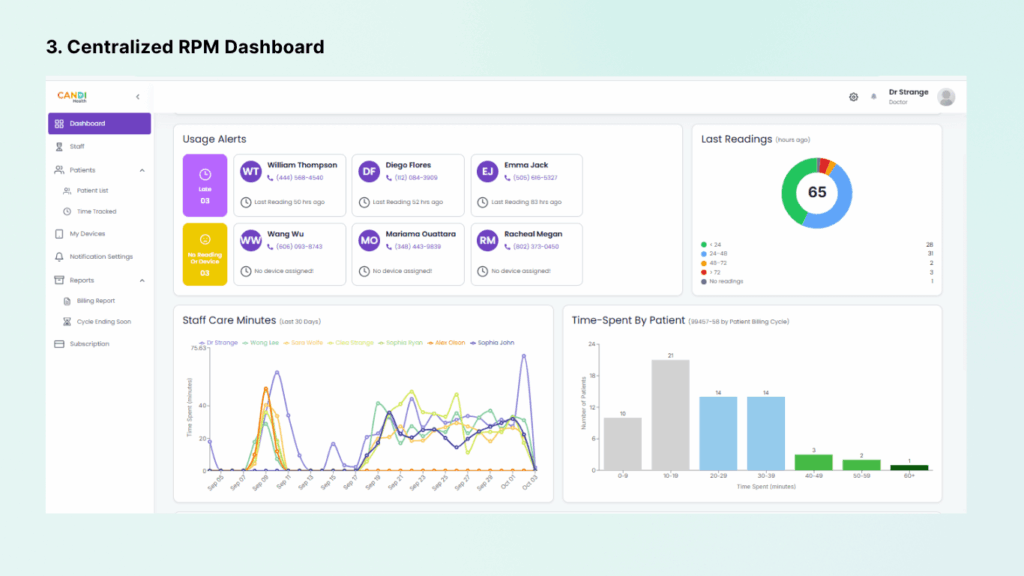
3. Centralized RPM Dashboard
All readings go into a secure, HIPAA-compliant dashboard. Staff can check blood pressure trends, see if patients are taking regular readings, and get alerts if numbers go out of range.
4. Automated Time Tracking and Reports
CandiHealth’s system keeps track of how much time staff spend reviewing data or contacting patients. It automatically calculates minutes for billing. With one click, you can generate audit-ready reports that show usage days, and care time. These reports are formatted for Medicare and insurers, so billing is simple and compliant.
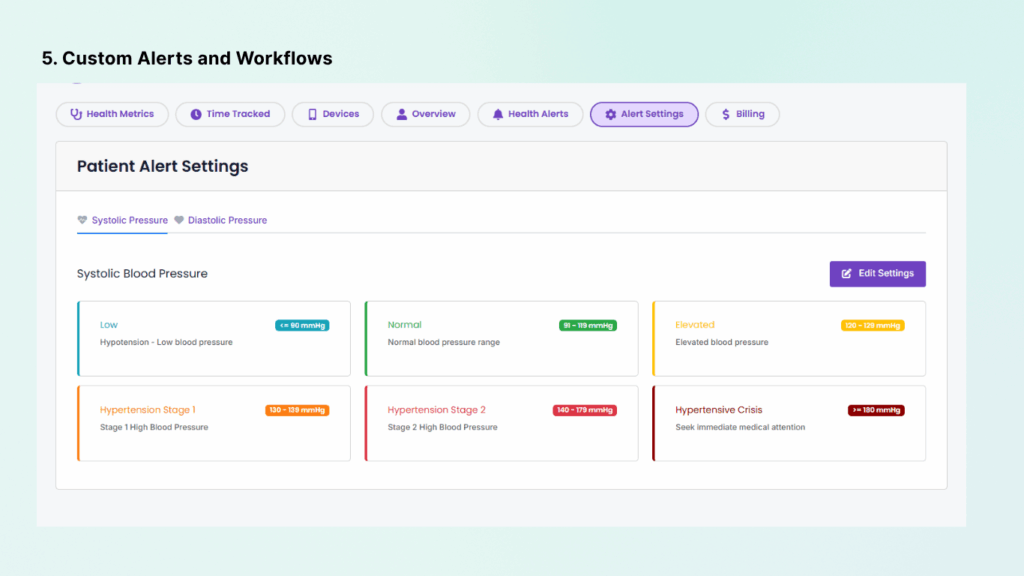
5. Custom Alerts and Workflows
Providers can set custom alert thresholds for each patient. For example, a heart-failure patient may need a lower alert limit. Alerts can also be assigned to specific staff, like a nurse or MA. This prevents alert overload and makes sure the right person gets notified. It keeps the team organized and focused.
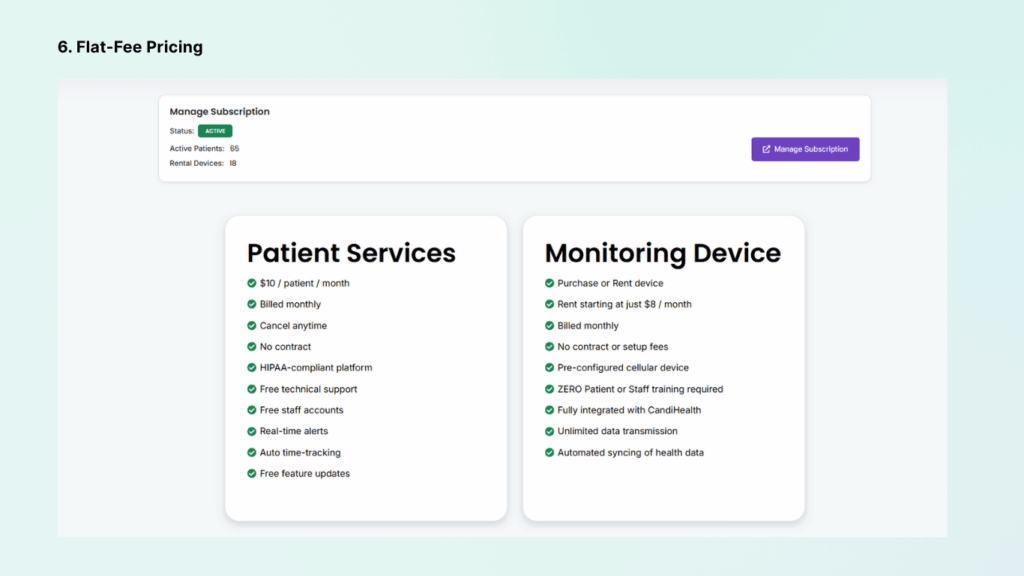
Flat-Fee Pricing
CandiHealth charges a flat $10 per patient per month for the platform. Devices can be purchased upfront or rented for about $10 per month each. There are no contracts or hidden fees. Clinics keep 100% of their RPM reimbursement. This clear pricing makes it easy to plan and protects your margins.
Support and Training
CandiHealth includes free technical support for both staff and patients. If a device has trouble, the support team helps fix or replace it. Devices can also be reset and reassigned to new patients in seconds. Training is provided through quick-start guides, video tutorials, and billing checklists. All systems follow HIPAA rules to keep patient data secure.
Eligibility Requirements to Start an RPM Program with CandiHealth
Before you start an RPM program, make sure you meet the following eligibility requirements:
- RPM must be ordered and overseen by a licensed provider. This includes physicians, nurse practitioners, and physician assistants.
- Medicare requires that the patient already has a relationship with the billing provider. You cannot bill RPM for someone you have never seen before.
- The patient must have a medical reason for monitoring, such as uncontrolled hypertension or other risk factors.
- Clinics should have staff ready to watch the data. Nurses or medical assistants can handle daily tasks under the provider’s supervision. Medicare allows this..
- Providers do not need to join a special program to use RPM. Any eligible provider can start, as long as they follow billing and compliance rules.
- Patients must give consent to join the program. This can be verbal or written but must be recorded in their medical file.
- Only one provider can bill RPM for a patient at a time. If a patient sees multiple doctors, they must enroll with the one managing their condition.
Read the following article for more information: RPM Billing Guidelines 2025: CPT Codes & Compliance Tips
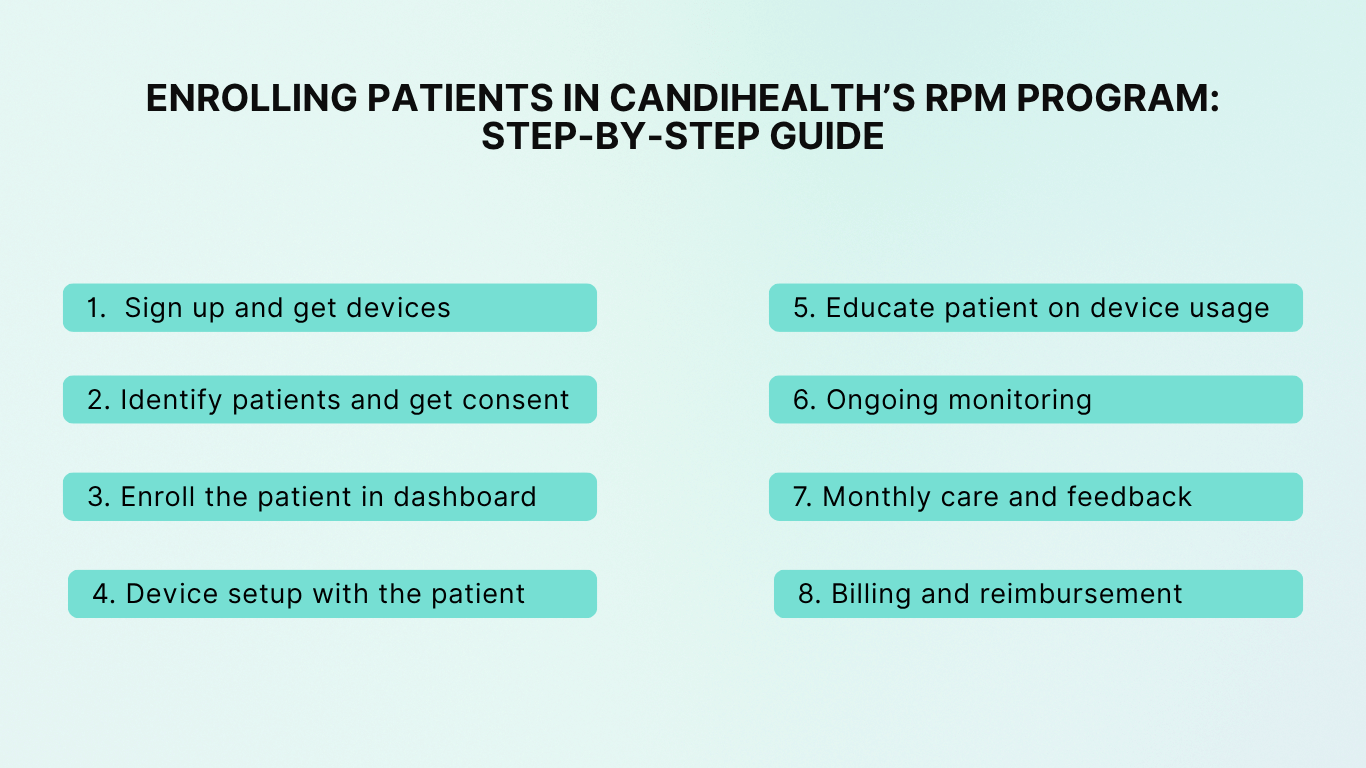
Enrolling Patients in CandiHealth’s RPM Program: Step-by-Step Guide
For clinics, getting a patient started with CandiHealth’s remote BP monitoring is simple. Below is a step-by-step guide that takes you from setup to billing.
- Sign up and get devices
- Identify patients and get consent
- Enroll the patient in dashboard
- Device setup with the patient
- Educate patient on device usage
- Ongoing monitoring
- Monthly care and feedback
- Billing and reimbursement
1. Sign Up and Get Devices
First, your clinic signs up for CandiHealth. This can be done online or after a short demo. You choose the flat-fee plan and decide whether to buy or rent devices.
CandiHealth then sends you pre-configured cellular BP cuffs. Each device is already linked to your clinic’s account. No IT setup is needed. You also receive login details for the clinic dashboard.
2. Identify Patients and Get Consent
Next, choose patients who will benefit most, those with uncontrolled BP, frequent visits, or high-risk conditions. Confirm they meet basic rules: they have a chronic condition, and they’re willing to take regular readings.
When you see them, explain the program in simple terms. Make sure the patient understands what’s expected, mainly, using the device often. Then get their consent, either verbal or written.
3. Enroll the Patient in the Dashboard
In the CandiHealth portal, create a new patient profile. Enter basic details (name, date of birth, etc.) and assign the device. Each cuff has a unique ID. Once it’s linked, all readings from that device will show up in the patient’s record automatically.
4. Device Setup With the Patient
Give the device to the patient in person or ship it to their home. Show them how to put on the cuff and press the Start button. No apps or Wi-Fi are needed.
If you see them in person, confirm the first reading appears in the system before they leave. If shipped, follow up by phone or telehealth to confirm it works. Also explain when to measure (e.g., once daily in the morning) and what to do if they get an alert reading.
5. Patient Education
Spend a few minutes teaching best practices:
- Sit quietly for a few minutes before measuring.
- Keep the cuff at heart level.
- Avoid caffeine right before taking a reading.
Reassure patients that your team will check the readings often. Let them know: “If your numbers are high or low, we’ll contact you. If you don’t hear from us, it means your readings are in a safe range.” This helps reduce anxiety and keeps trust.
Read: How to Use Remote Patient Monitoring Devices at Home?
6. Ongoing Monitoring
Once enrolled, your clinic workflow begins. The CandiHealth dashboard shows all readings in real time. Staff can log in daily or at set times to review.
You can set alert thresholds for each patient. If readings cross that line, the system notifies the assigned staff member. That nurse or MA can then call the patient, check symptoms, and follow your protocol.
Even if readings are normal, staff should check compliance (e.g., if a patient hasn’t used the cuff in days, someone should remind them).
7. Monthly Care and Feedback
Medicare requires at least 20 minutes of RPM-related care each month. This includes reviewing data, phone calls, care plan changes, and documentation.
A good workflow is to set aside time each week for RPM check-ins. Staff can review readings, call patients, and log time. Patients must also get at least one interactive communication each month, like a quick phone call or telehealth check-in.
For example: “Hi, I’m calling about your blood pressure readings this month. Most were in range, but a few were high. How are you feeling?” These conversations help patient care and fulfill billing rules.
8. Billing and Reimbursement
At the end of each month, generate claims with the CandiHealth report. The system shows which codes are billable:
- 99453 – one-time setup and training
- 99454 – device supply and 16+ days of readings
- 99457 – first 20 minutes of care
- 99458 – each extra 20 minute
The platform tracks everything and prepares audit-ready reports. Claims go through your normal billing process. Medicare and many private payers reimburse for these codes.
Enrolling patients in CandiHealth’s RPM program follows a clear path: sign up, identify patients, get consent, assign devices, educate, monitor, and bill. After the first few patients, the process becomes routine and can scale to dozens. CandiHealth’s support team helps along the way, making RPM a smooth addition to your clinic’s care.
Technical and Staffing Requirements for Implementation
To run a remote BP monitoring program smoothly, a clinic needs both the right tools and the right team. CandiHealth is built to keep tech barriers low, but there are still a few basics to cover.
Technical Requirements
Technical requirements include the following:
- Internet and computer access.
- Medical devices (BP monitors)
- Data security and HIPPA-compliance
Here is a brief description of each.
1. Internet and Computer Access
Your staff will need a computer or tablet with internet access. The CandiHealth dashboard is cloud-based and works in a normal web browser. No special hardware is required. Just make sure your internet is stable and that staff can log in securely.
2. Devices (BP Monitors)
CandiHealth provides cellular blood pressure cuffs. Keep devices in a safe place at the clinic, and have a plan for handing them out or collecting them back. It’s also smart to keep a few extras on hand as backups. If a device stops working, CandiHealth’s support team will help with a replacement.
3. Data Security and HIPAA Compliance
All patient data is handled securely through CandiHealth’s HIPAA-compliant system. Each staff member should have their own login. You can assign roles, for example, nurses can add notes and time logs, while billing staff can just view reports. Train staff to log out when done and to avoid downloading patient data to personal devices.
Staff and Workflow Requirements
A remote blood pressure monitoring program is only as strong as the people running it. With CandiHealth, the technology is simple, but success depends on setting up clear roles, training your staff, and making RPM part of your daily care.
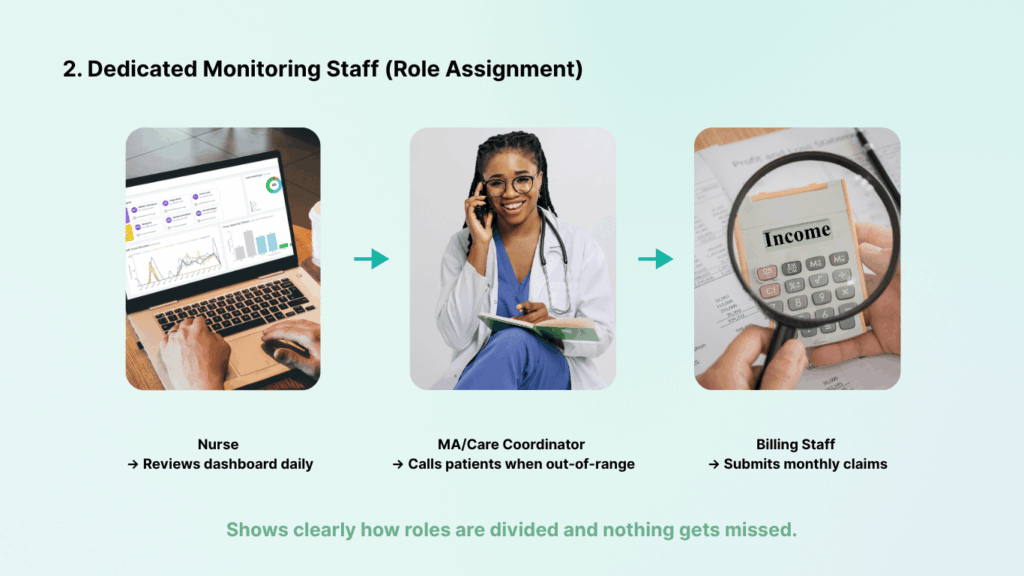
1. Dedicated Monitoring Staff (Role Assignment)
While you likely won’t need to hire new staff solely for RPM (especially when starting small), you do need to allocate existing staff time to manage the program. Typically, a nurse, medical assistant, or care coordinator can be responsible for RPM duties.
The key is to clearly define roles and responsibilities. Decide who will review the daily BP readings and alerts. Decide who will contact patients when readings are out of range . Also decide who will handle documentation and billing prep.
Ensure management coverage for when staff are out – e.g., have a backup person who knows how to use the system if the primary nurse is on vacation. The goal is that no alert or important trend goes unnoticed, and that required patient interactions (monthly calls) occur reliably.
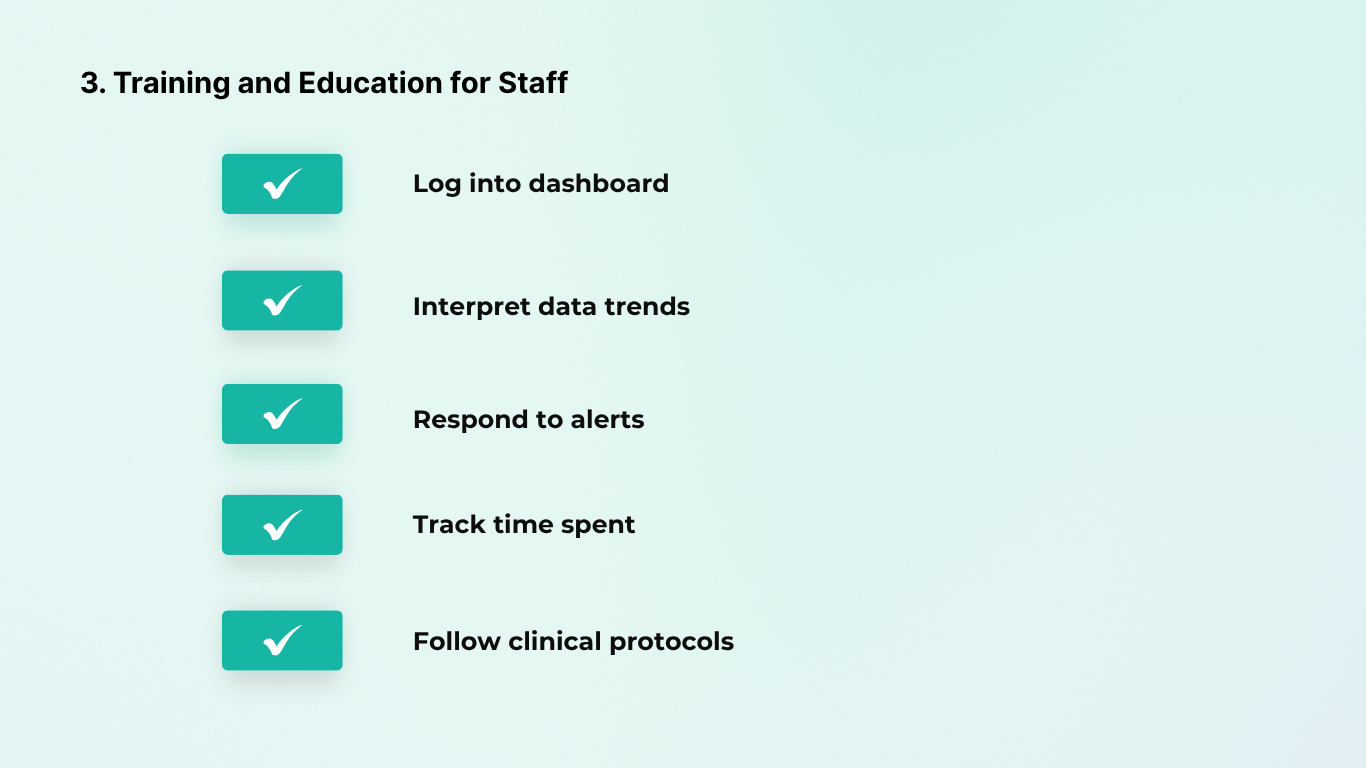
2. Training and Education for Staff
Your clinical staff will need some initial training on using the RPM program. CandiHealth makes this relatively quick by providing training videos and guides. However, plan a training session where staff learn how to: log into the dashboard, interpret the data, respond to alerts, and mark time spent on activities. In addition, staff should be educated on clinical protocols.
For instance, establish a protocol like “If 3 consecutive readings >180 systolic, do X” or “If patient’s BP is in hypertensive urgency range, notify Dr. Smith immediately.” Having clear clinical guidelines will help staff act consistently. CandiHealth’s support team is on hand if your staff have questions; don’t hesitate to use them, especially early on.
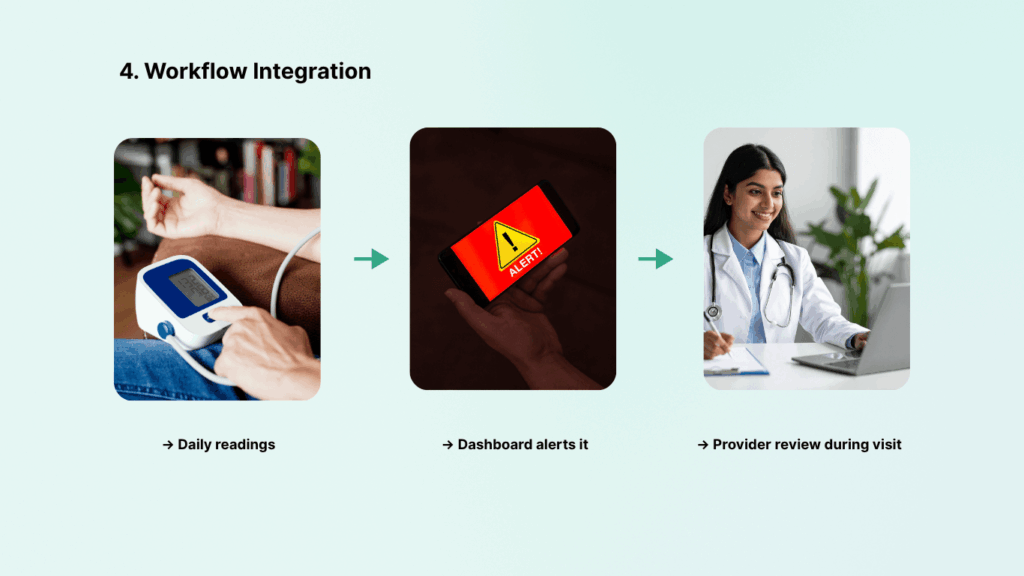
3. Workflow Integration
Treat the RPM program as an extension of your patient care by incorporating RPM checkpoints into your existing workflows. For example, when a patient comes in for an office visit, the provider can pull up their RPM dashboard or recent summary to discuss trends.
In the clinic’s daily schedule, you might include a quick “RPM huddle” or check during morning rounds. Setting up a regular schedule can help you stay on track. CandiHealth’s alert system will proactively prompt staff for urgent issues, but consistent routine follow-up is needed for non-urgent monitoring as well.
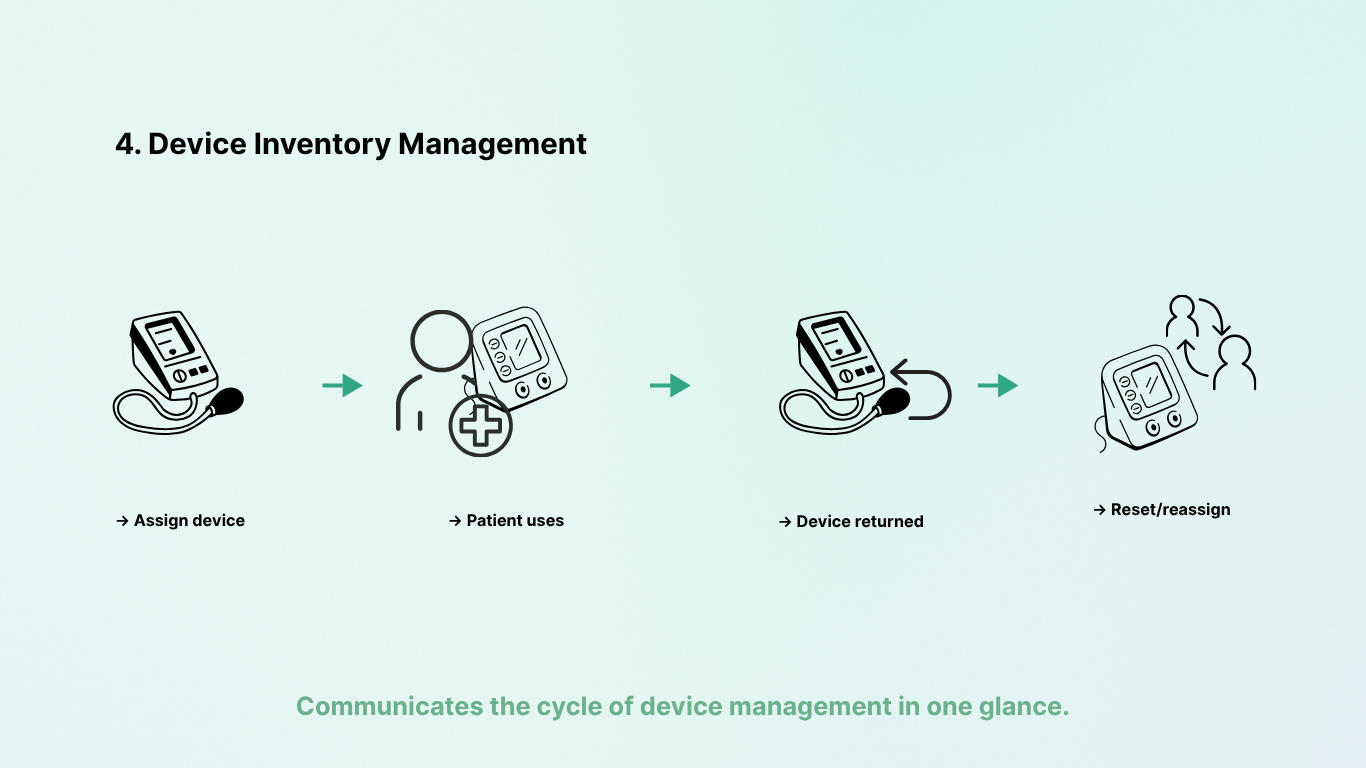
4. Device Inventory Management
Operationally, designate someone to keep track of the RPM devices. This includes logging which patient has which device (the CandiHealth portal does this mapping when you assign devices, but you may also want a simple spreadsheet or inventory list). If a patient leaves the practice or stops the program, you should retrieve their device (if possible) so it can be reassigned.
CandiHealth makes reassignment easy (resetting the device in the portal), but you need to physically have the device. Thus, having a process for device pickup or mailing return labels is useful.
5. Scaling Up Staffing as Program Grows
In the beginning, if you only enroll, say, 5-10 patients, your existing nurse can handle this easily in addition to normal duties. As the program grows to dozens or hundreds of patients, you may need to allocate more staff time or hire additional help.
Many practices find that for roughly every 100-150 RPM patients, you might need about 0.5 to 1.0 full-time equivalent (FTE) of a nurse or care coordinator to manage the load..
CandiHealth Vs.Other Remote Patient Monitoring Platforms
Remote patient monitoring for blood pressure management is a growing field, and there are several reputable service providers and models available in the U.S. healthcare market. It’s useful to understand how CandiHealth’s approach compares with other major RPM services, so providers can make an informed choice. Below, we outline some key points of comparison, highlighting a few notable RPM programs:
1. Full-Service RPM vs. Self-Managed RPM
Some companies offer full-service RPM solutions that include their own clinical monitoring staff and hands-on management. For example, Accuhealth provides a 24/7 nurse-staffed monitoring center that watches incoming data around the clock and can even handle patient outreach on your behalf.
These full-service options reduce the burden on your staff, but you have to share a portion of reimbursement or pay higher fees for the added services.
In contrast, CandiHealth empowers the clinic’s own team with easy-to-use tools rather than replacing them. CandiHealth keeps the provider in control of clinical workflows and does not offer staff to manage your patients. This is ideal for practices that want to maintain direct relationships with patients and retain all the RPM revenue.
2. Device Connectivity and Patient Technology
Virtually all leading RPM programs now use cellular-connected devices for monitoring vitals like blood pressure, because it drastically lowers the technical barrier for patients. CandiHealth is fully in line with this trend (cellular, pre-configured devices). A difference to note is that a few platforms support Bluetooth device options as well, for clinics or patients who might already have a device.
CandiHealth and most modern competitors recognize that simplicity is key: an RPM program won’t succeed if patients can’t get the device to transmit data. CandiHealth’s strict “no smartphone needed” policy is matched by players like HealthSnap, Accuhealth, Athelas, etc., all of whom ship devices ready to use. So in terms of device tech, CandiHealth is on par with the top services using plug-and-play blood pressure cuffs.
3. RPM Pricing and Revenue Model
RPM vendors use different pricing models. Some enterprise-level solutions charge health systems large setup fees or per patient per month fees plus a share of reimbursement. HRS (Health Recovery Solutions), for example, often works with hospitals and may have more customized pricing for its comprehensive platform (including telehealth tablet kits, etc.).
CandiHealth’s flat $10 per patient per month platform fee with no contract and no revenue sharing is very straightforward. For a typical clinic looking at cost: CandiHealth’s model means you pay a fixed predictable amount and keep the rest.
Some other vendors might say “we will do everything and split the reimbursement 80/20” or might charge, say, $30–$60 per enrolled patient per month but handle more tasks.
Evaluate whether you want a turnkey service at higher cost or a lightweight service at lower cost. CandiHealth clearly positions itself as low-cost and transparent – “no hidden fees” making it attractive to clinics that want to maximize their RPM profit and avoid surprise bills.
4. Service and Support Offerings
Another differentiator is the extent of support services. Some RPM companies provide robust patient engagement services. For example, HealthSnap doesn’t just send devices; they also handle patient outreach, enrollment, adherence monitoring, and even some billing work for the provider.
In comparison, CandiHealth’s support is highly responsive for technical issues and onboarding, and they provide training resources. But clinical coaching or routine patient outreach is left to the clinic. CandiHealth’s philosophy is to keep things simple: they solve the tech and process hassles, and you handle the care (which many providers prefer).
Many smaller practices find that with CandiHealth, their existing staff can manage and they value that CandiHealth isn’t coming between them and their patients – it’s just facilitating their interaction.
Why Choose CandiHealth for Remote Patient Monitoring?
Every clinic is different. Some want outside support teams to run remote monitoring. Others prefer to keep care in-house but need tools that don’t add more work. The right choice depends on your staff, your patients, and the way you already deliver care.
1. Full-Service Models
There are programs where an outside company manages most of the monitoring. These services often provide their own nurses and handle patient calls. They can be helpful for large hospital systems or patients with very complex needs.
But they also come with trade-offs: higher costs, less direct control, and in some cases, revenue sharing.
2. In-House Platforms
Other programs give clinics the tools but leave the work fully on your staff. These often rely on apps, Wi-Fi, or extra setup at the patient’s home. They can work well for tech-savvy patients, but they may be harder to manage in busy practices with limited staff time.
So, How CandiHealth is Best for You?
CandiHealth is built for clinics that want the middle ground: control stays in your hands, but the hard parts are removed.
- Devices work out of the box with no apps or Wi-Fi.
- Pricing is flat and predictable, with no revenue cuts.
- The dashboard is simple and easy to use.
Choosing What Works Best for You
Some large systems may decide to mix programs — one for patients needing daily nurse calls, another for routine hypertension monitoring. But for most outpatient practices, especially in primary care and cardiology, a single program that is easy to use and reliable is often enough.
If your goal is straightforward, to track blood pressure, support patients, and bill with confidence, CandiHealth is designed to meet that need without adding complexity. It keeps things simple, lets your team stay in control, and helps you focus on what matters most: patient care.