Table of Contents
Imagine this: A patient checks their blood pressure each morning. A reading outside their normal range triggers an alert. Their nurse reviews the data, makes a call, and adjusts their medication accordingly, without waiting for the next clinic visit.
This is the power of remote patient monitoring—a technology-driven approach that bridges the gap between home and healthcare facilities. And the devices patients use to measure and send their health data, are called remote patient monitoring (RPM) devices.
By measuring and transmitting vitals like blood pressure, weight, or oxygen saturation from home, these devices help care teams stay connected to patients even when they’re not physically present. And as remote care becomes a standard part of chronic disease management, it is important to understand how these devices work.
This guide covers the most common RPM devices in remote patient monitoring, how they work, and where they fit into everyday clinical routines.
What Are Remote Patient Monitoring Devices?
Remote patient monitoring devices are used to track vital health data outside of traditional clinical settings. These devices allow healthcare professionals to monitor vital signs like blood pressure, glucose levels, weight, heart rate, and oxygen saturation in real time or at set intervals.
They play a critical role in managing chronic conditions such as hypertension, diabetes, heart failure, chronic obstructive pulmonary disease (COPD), and asthma. Depending on the condition, patients may use these devices daily or multiple times a week.
The data collected is securely transmitted, typically through Bluetooth, Wi-Fi, or cellular networks, to healthcare providers. This helps clinicians identify trends, detect problems early, and take necessary action before a patient ends up in the ER.
How Do RPM Devices Improve Outcomes?
The key advantage of RPM lies in early detection and intervention.
For instance, a sudden spike in blood pressure, an unexpected drop in oxygen levels, or a steady weight increase can signal underlying issues. Without RPM, such changes might go unnoticed until a routine appointment or an emergency arises.
By tracking these metrics consistently, RPM devices allow care teams to:
- Adjust medications quickly
- Schedule follow-ups at the right time
- Avoid unnecessary hospitalizations
- Improve chronic disease management
This not only helps patients feel more supported but also reduces stress, enhances quality of life, and minimizes the financial burden associated with avoidable hospital stays.
How Do RPM Devices Transmit Data?
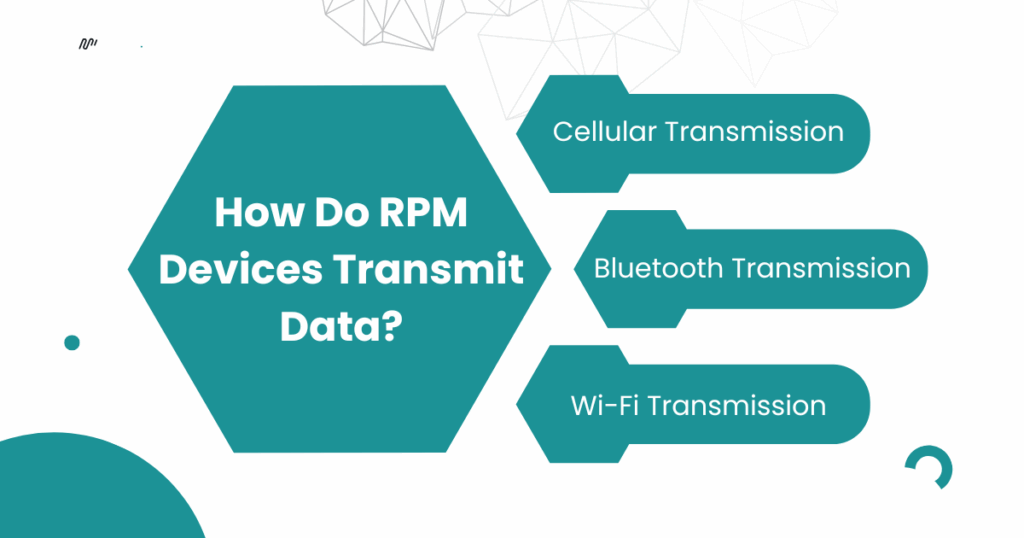
Remote patient monitoring devices are only effective if they can reliably share patient data with care teams in a secure and timely manner. That’s why data transmission is a core feature of any RPM system, and it’s designed to be simple for patients, yet powerful for providers.
Most RPM devices transmit data through one of three common methods:
1. Cellular Transmission
Some RPM devices come with built-in cellular connectivity, similar to a mobile phone. These devices don’t require a smartphone or Wi-Fi network. They transmit data automatically using a secure cellular signal.
Cellular devices are suitable for:
- Elderly patients or those without internet access
- Rural areas with limited Wi-Fi infrastructure
- Plug-and-play experience with no setup required
Examples:
- Blood pressure monitors with embedded SIMs
- Digital weight scales with LTE connectivity
Many modern care platforms, like CandiHealth, are now prioritizing cellular-first models to remove technical barriers and increase patient adherence.
2. Bluetooth Transmission (Paired with Smartphone or Tablet)
Many modern RPM tools connect via Bluetooth to a companion mobile app on the patient’s smartphone or tablet. The app then transmits the collected data to the healthcare provider’s system over the internet.
These devices are suitable for:
- Tech-savvy patients
- Programs that require interactive mobile apps
- Devices like CGMs, ECG patches, and oximeters
Considerations:
- Requires patient to keep Bluetooth and Wi-Fi enabled
- May involve syncing steps or app permissions
3. Wi-Fi Transmission
Some devices connect directly to the patient’s home Wi-Fi network to transmit data to the cloud. These are often used in homes where patients have stable internet access and can connect the device to their network during setup. These devices are best for:
- Daily monitoring in digitally connected households
- Devices that require regular firmware or software updates
Is the Data Secure?
Yes. All RPM data is transmitted using end-to-end encryption and stored in HIPAA-compliant systems. Whether using cellular, Bluetooth, or Wi-Fi, data is encrypted both in transit and at rest to protect patient privacy and comply with healthcare regulations.
Integration with Clinical Systems
Once received, RPM data can be:
- Sent to a clinical dashboard for review
- Integrated with Electronic Health Records (EHRs) like Epic or Cerner
- Highlighted by automated alerts or AI triage systems for abnormal readings
Common Remote Patient Monitoring Devices
RPM devices are assigned based on the condition being managed, whether it’s blood pressure, blood glucose, or respiratory function, and are selected for both clinical accuracy and ease of use at home.
Here’s a closer look at the most widely used devices in remote patient monitoring.
1. Blood Pressure Monitors
Blood pressure monitors are among the most widely used RPM devices, especially for patients managing hypertension, cardiovascular disease, or post-stroke care.
These devices typically use an upper-arm cuff to measure systolic and diastolic pressure. The results are transmitted automatically to healthcare teams via Bluetooth or cellular networks, eliminating the need for manual logs.
In most programs, patients are asked to take readings once or twice daily, often in the morning. Devices used in RPM are designed with user-friendly interfaces, large displays, and automatic transmission features to ensure seamless data sharing.
Over time, these readings help providers identify patterns, catch early warning signs of complications, and adjust medications more accurately.
2. Glucose Monitoring Devices
For individuals living with diabetes, daily glucose monitoring is critical. In RPM programs, this is typically done through either:
- Fingerstick glucometers, which require a small blood sample
- Continuous glucose monitors (CGMs), which use a sensor placed under the skin to provide ongoing glucose readings
While fingerstick devices often require patients to input readings manually, CGMs offer automatic, real-time data sharing. This allows clinicians to see glucose trends over time.
CGMs are especially beneficial in remote care because they:
- Improve glycemic control
- Reduce hypoglycemic events
- Provide insights into how food, stress, and medication impact blood sugar
By integrating CGM data into care plans, providers can offer personalized feedback and make timely adjustments, without waiting for the next appointment.
3. Pulse Oximeters
A pulse oximeter is a small, non-invasive device that clips onto a patient’s finger to measure oxygen saturation (SpO2) and pulse rate.
These devices are especially valuable for patients with respiratory conditions such as COPD, asthma, or post-COVID symptoms, where oxygen levels may fluctuate without obvious symptoms.
In RPM, pulse oximeters are typically used on a daily basis or during specific symptom episodes. Some programs also use them for early detection of silent hypoxia—a condition where oxygen levels drop before a patient feels short of breath. Readings outside of normal ranges can trigger clinical alerts and prompt follow-up care.
4. Digital Weight Scales
For patients managing congestive heart failure (CHF), kidney disease, or metabolic conditions, weight monitoring is important.
A daily increase of even 2–3 pounds can signal fluid retention, which may indicate worsening heart failure. That’s why many RPM programs include digital scales that automatically transmit weight readings to providers.
Unlike typical home scales, RPM-enabled scales:
- Detect subtle weight fluctuations
- Sync data instantly via cellular or Bluetooth
- Are often pre-configured for ease of use
Early identification of weight trends enables care teams to intervene before symptoms escalate, preventing ER visits and improving long-term outcomes.
5. ECG and Heart Rate Monitors
Providers use ECG monitors to track heart rhythms in patients with arrhythmias, atrial fibrillation, or those recovering from cardiac procedures. These devices may come as chest straps, skin patches, or handheld sensors.
Some tools collect and send ECG data in real time. Others store the data and upload it periodically. Either way, they help care teams detect irregular patterns, verify patient-reported symptoms, and monitor recovery progress without requiring in-person visits.
6. Spirometers and Peak Flow Meters
Spirometers measure lung function by recording the volume and speed of air a patient can inhale and exhale. They are most commonly used in remote care programs for patients with chronic respiratory diseases such as asthma, COPD, or pulmonary fibrosis.
Some programs also use simpler peak flow meters, which focus on measuring the patient’s maximum exhalation speed. These tools help track lung health trends over time and can alert care teams to early signs of deterioration.
While not as widely used as BP or glucose monitors, they are an important part of RPM for respiratory patients.
7. Thermometer
In remote care programs that involve infection monitoring, post-surgical recovery, or chronic inflammatory conditions, digital thermometers play an important role.
These devices help track body temperature consistently and alert providers to early signs of fever.
While many patients already own standard thermometers, RPM-enabled versions automatically log and send readings to the care team.
This eliminates the need for manual tracking and allows providers to monitor trends over time, especially useful when managing immunocompromised patients, those recovering from surgery, or individuals with autoimmune conditions.
Are These Devices Clinically Approved and Regulated?
When health decisions are being made based on data collected outside traditional settings, it’s essential that the devices involved are not only accurate, but also clinically approved and regulated.
That’s why most remote patient monitoring (RPM) devices used in care programs undergo rigorous safety and performance evaluations before they ever reach a patient’s home.
Are RPM Devices FDA-Approved?
In the United States, most RPM devices are reviewed and cleared by the Food and Drug Administration (FDA), particularly those classified as medical-grade and used in reimbursable programs.
These include:
- Blood pressure monitors
- Glucometers and continuous glucose monitors (CGMs)
- Pulse oximeters
- ECG patches and handheld monitors
- Spirometers and smart thermometers
The FDA typically classifies RPM devices as Class II medical devices, which means they are moderate-risk but require special controls to ensure their effectiveness. Manufacturers must demonstrate performance accuracy, usability, and data integrity before these devices are allowed on the market.
Why Regulatory Approval Matters
For healthcare providers, FDA clearance ensures that the data collected remotely is reliable enough to guide clinical decisions, like medication adjustments or emergency interventions.
For patients, it offers peace of mind. They can trust that the device they’re using at home meets the same quality standards as tools used in clinics or hospitals.
Frequently Asked Questions (FAQs)
1. What are remote patient monitoring systems?
Remote patient monitoring (RPM) systems are a combination of medical devices and digital platforms that collect, transmit, and store a patient’s health data from home to their healthcare provider. These systems allow for continuous tracking of vitals like blood pressure, glucose levels, and oxygen saturation without requiring in-person visits.
2. What devices are used for RTM?
Remote Therapeutic Monitoring (RTM) typically involves devices that track non-physiological data, such as musculoskeletal motion, respiratory patterns, and therapy adherence. Common RTM devices include respiratory monitors, wearable motion sensors, and apps that collect therapy engagement data.
3. Which technology is used for remote patient monitoring?
RPM uses a mix of technologies including cellular networks, Bluetooth, and Wi-Fi for data transmission. Devices are often connected to cloud-based dashboards and integrate with Electronic Health Record (EHR) systems. Many modern RPM platforms also use AI and automation to triage data and highlight abnormal readings.
4. Can you give remote patient monitoring devices examples?
Yes, here are common examples of FDA-cleared remote patient monitoring devices:
- Blood pressure monitors
- Continuous glucose monitors (CGMs)
- Digital weight scales
- Pulse oximeters
- ECG patches or handheld monitors
- Spirometers and peak flow meters
- Connected thermometers
These devices are selected based on the patient’s condition and transmit health data securely to care teams for review.
Final Thoughts
Remote patient monitoring devices help doctors catch issues early, give patients more control at home, and reduce the need for unnecessary visits. From managing blood pressure and blood sugar to tracking oxygen levels and weight, these tools make it easier to stay on top of everyday health needs.
But for remote care to really work, the devices have to be simple for patients to use, and reliable enough for providers to act on. That’s where the right platform makes a difference.
At CandiHealth, we keep things straightforward. Our devices are ready to go out of the box, work without Wi-Fi or smartphones, and are built for people who just want things to work.
Looking to simplify RPM for your patients? Get in touch with us to see how we can help.