Remote Patient Monitoring (RPM) is changing how patients receive care, especially for those managing chronic conditions like hypertension or diabetes. Yet, despite its growing adoption, many patients still hesitate to embrace it—often because of misunderstandings or outdated perceptions.
Some think RPM is complicated. Others fear it’s costly, impersonal, or even unsafe. In reality, RPM makes healthcare more accessible and proactive. It allows doctors to monitor patients’ vital signs, right from home using connected devices.
According to the American Medical Association, over 76% of U.S. hospitals now use RPM technologies, proving how trusted and mainstream it has become.
Still, misconceptions persist. These myths can prevent patients from taking advantage of a tool that can actually make their lives easier and safer.
This blog breaks down the five most common myths patients have about remote patient monitoring and reveals what’s true—so you can make informed decisions about your health.
What Are the 5 Myths Patients Have About Remote Patient Monitoring?
Remote Patient Monitoring (RPM) is one of the simplest, safest, and most patient-friendly ways to stay connected with your healthcare team. It doesn’t replace your doctor; it simply extends their care to your home. Using smart devices—like a cellular blood pressure monitor or glucose meter—your readings are automatically sent to your care team. If anything looks unusual, your doctor can follow up right away.
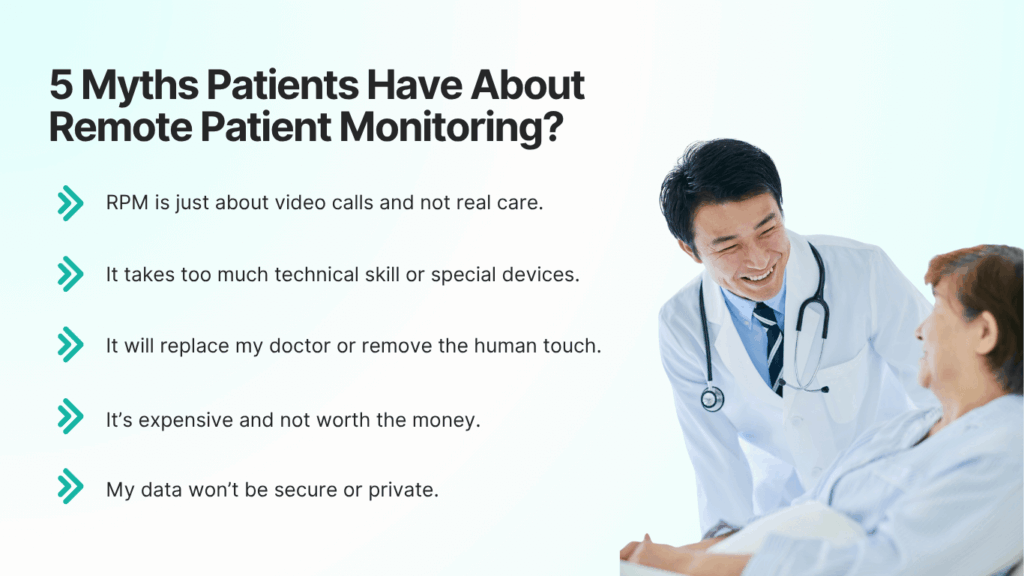
Yet, despite how effective and easy it is, patients still hold onto a few persistent myths. The most common ones include:
- RPM is just about video calls and not real care.
- It takes too much technical skill or special devices.
- It will replace my doctor or remove the human touch.
- It’s expensive and not worth the money.
- My data won’t be secure or private.
Let’s break them down one by one.
Myth 1: RPM is Just About Video Calls and Not Real Care
This is one of the most common misunderstandings. Many patients confuse Remote Patient Monitoring (RPM) with telehealth visits. While both use technology to connect patients and providers, they serve different purposes.
- Telehealth involves virtual consultations—video or phone calls between you and your doctor.
- RPM, on the other hand, continuously collects your health data from home through smart medical devices and securely transmits it to your care team.
That means instead of occasional check-ins, your health is monitored daily. For example:
- A cellular BP monitor records your blood pressure every morning.
- The reading automatically uploads to your clinic’s dashboard.
- If the numbers rise above normal, your care team gets an alert and contacts you right away.
A study published in the Journal of the American Heart Association found that RPM programs reduced hospital readmissions by up to 25% for chronic disease patients. That’s because care becomes proactive, not reactive.
Myth 2: It Takes Too Much Tech Skill or Devices Are Too Complex
Another common belief is that remote patient monitoring sounds too “high-tech” for everyday patients—especially seniors. Many imagine having to install apps, connect Wi-Fi, or troubleshoot complicated software. This fear of technology keeps some patients from ever trying RPM in the first place.
In reality, modern RPM systems are designed for simplicity. Most patients only need to use one or two small medical devices, such as a cellular blood-pressure monitor or Bluetooth glucose meter. These devices automatically send readings to the care team—no smartphone pairing, app downloads, or Wi-Fi setup required.
According to a 2023 report by the National Library of Medicine, over 82% of seniors successfully used RPM devices after a short orientation call—proving that user-friendliness is at the heart of modern RPM design.
Pro Tip for Patients: When signing up for an RPM program, ask whether your device is cellular-enabled (not Wi-Fi dependent). Cellular devices, like those offered by CandiHealth, arrive pre-connected and ready to use right out of the box—making them ideal for patients of all ages.
Myth 3: It Will Replace My Doctor or Remove the Human Touch
RPM doesn’t replace your physician; it gives them better visibility into your daily health. Instead of waiting for your next appointment, your doctor can see how your condition is progressing in real time. For example, if your blood pressure readings spike, your care team can reach out immediately rather than discovering it weeks later during a clinic visit.
According to a 2024 study by the American College of Cardiology, patients using RPM for chronic conditions were 30% more likely to report feeling “connected” to their care teams than those who relied solely on traditional visits. That’s because they received personalized feedback and quicker follow-ups.
Think of it this way:
- Without RPM: You see your doctor every few months and share a few readings or symptoms from memory.
- With RPM: Your doctor sees how your numbers change every day, understands patterns, and adjusts your treatment faster.
Myth 4: It’s Too Expensive / I’ll Have to Pay a Lot
Many patients assume remote patient monitoring must be costly because it uses connected medical devices. The truth? RPM is usually covered by Medicare and most insurance plans, especially for chronic conditions like high blood pressure or diabetes.
In most cases, you don’t pay anything extra. Your clinic bills Medicare using standard CPT codes (99453, 99454, 99457, 99458), so the service is reimbursed just like a regular doctor visit.
RPM also helps you save money in the long run. By catching early signs of health issues, it prevents ER visits and unnecessary trips to the clinic. For example:
| Expense Type | Without RPM | With RPM |
| ER visits | More frequent | Fewer visits due to early alerts |
| Travel costs | Regular clinic trips | Remote monitoring from home |
| Device cost | Often extra | Usually included in the program |
CandiHealth partners with clinics under a flat-fee model, meaning there are no hidden patient costs or surprise fees. You simply use the device, and your care team handles the rest.
Myth 5: My Data Won’t Be Secure or Private
Every RPM provider that works with clinics in the U.S. must follow HIPAA (Health Insurance Portability and Accountability Act) regulations. This law ensures that your medical data is encrypted, stored securely, and only shared with your authorized care team. Here’s how your data stays safe:
- Encrypted Transmission: All readings are sent through secure, encrypted channels.
- Limited Access: Only your doctor and clinical staff can view your health data.
- Regular Monitoring: Systems are continuously checked for security and compliance.
- No Third-Party Sharing: Your data isn’t shared or sold for marketing purposes.
According to a 2024 study by the Office for Civil Rights (OCR), RPM systems with built-in encryption had zero reported data breaches among compliant providers over the past two years—showing how robust these protections are.
CandiHealth Tip: CandiHealth follows full HIPAA compliance, encrypts all transmissions, and uses secure U.S.-based servers to protect your privacy. You stay in control of your health data—always.
Why These Myths Persist & What to Ask Your Provider
Even though remote patient monitoring is becoming common in clinics across the U.S., some of these myths still linger. The main reason is lack of awareness—many patients have never used RPM or confuse it with older telehealth systems. Some had frustrating tech experiences in the past, while others simply haven’t seen how far modern healthcare technology has come.
- Old stories about complicated tech.
- Fear of extra costs or hidden fees.
- Worry about losing the personal doctor connection.
- Little awareness about Medicare coverage.
When your doctor recommends a remote monitoring program, a few simple questions can help you feel confident and informed:
- What devices will I use, and are they easy?
- Does insurance or Medicare cover this?
- Who can see my data?
- How will my doctor respond to unusual readings?
- What happens if I need help using the device?
Final Thoughts
Remote Patient Monitoring is a simple way to stay healthier with the support of your care team. By understanding the truth behind these five common myths, you can make decisions based on facts. RPM doesn’t replace your doctor, add extra costs, or require advanced tech skills. Instead, it helps you stay on track, avoid unnecessary clinic visits, and get timely support when your readings change.
If your provider recommends RPM, ask questions, learn how it works, and see how it can fit into your daily routine. With the right program, remote monitoring becomes one of the easiest steps you can take to stay safe, informed, and in control of your health, right from home.
Considering RPM? Ask Your Doctor About CandiHealth
If you’re thinking about joining a remote monitoring program, it’s worth asking your doctor what system they use. Many clinics choose CandiHealth because it’s simple for patients—no apps, no Wi-Fi, and no complicated steps.
CandiHealth’s cellular blood pressure devices come pre-configured, so all you do is take your reading. Your numbers are sent securely to your care team, and they’re notified if anything needs attention. It’s an easy way to stay connected to your doctor between visits without changing your routine.
If your clinic works with CandiHealth, you’ll get a straightforward experience designed to keep you safe, supported, and informed—right from home.
FAQs About Remote Patient Monitoring
1. Is Remote Patient Monitoring safe to use at home?
Yes. RPM uses HIPAA-compliant systems and encrypted networks to protect your data. Only your healthcare team can access your readings.
2. Does insurance or Medicare cover Remote Patient Monitoring?
In most cases, yes. Medicare and many insurance plans fully cover RPM for chronic conditions like hypertension and diabetes under CPT codes 99453–99458.
3. Will I need Wi-Fi or a smartphone to use RPM devices?
No. Most modern RPM devices, like those from CandiHealth, are cellular-enabled, so they send readings automatically—no apps or Wi-Fi required.
4. Can Remote Patient Monitoring replace in-person doctor visits?
No. It complements your regular visits by keeping your doctor informed between appointments, helping catch changes early.
5. What if I’m not tech-savvy?
That’s okay. RPM devices are designed for ease of use, just take your reading, and the data is sent automatically.