Nearly 80% of older adults in the U.S. live with at least one chronic condition, and many struggle to track their health between clinic visits. Remote patient monitoring seems like a solution, but its dependence on smartphones and Wi-Fi often makes simple tasks harder, especially for elderly patients.
That’s why cellular RPM devices are gaining popularity. These tools send readings straight to the care team through built-in cellular networks. No apps or Wi-Fi needed. For seniors who find technology overwhelming, this makes daily monitoring far less stressful.
But the real question is: do cellular RPM devices actually improve health? In this blog, you’ll learn the benefits of cellular RPM devices for elderly patients, from reducing hospital visits to giving families peace of mind.
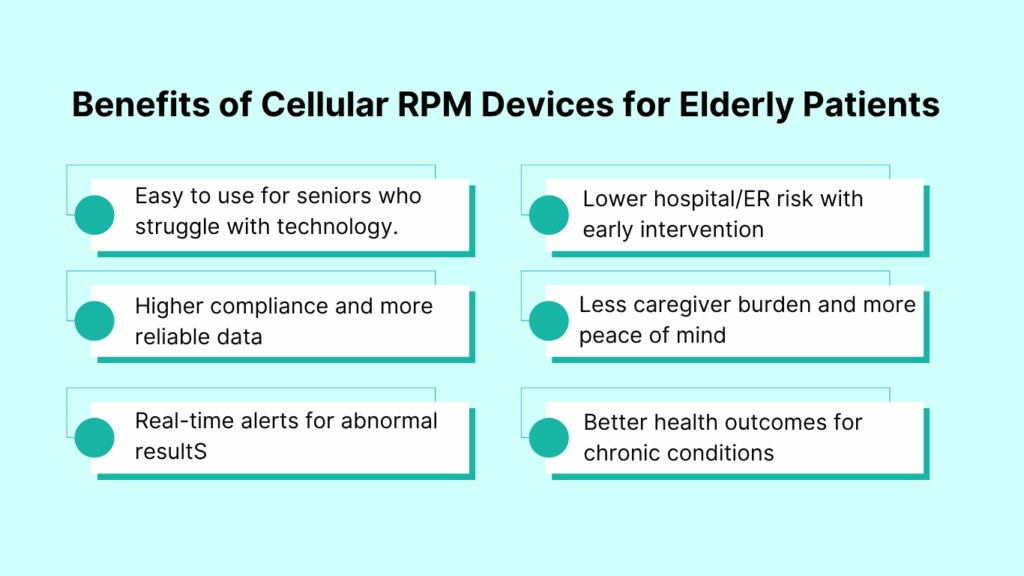
Benefits of Cellular RPM Devices for Elderly Patients
Cellular RPM devices help elderly patients by removing Wi-Fi and smartphone barriers, improving daily compliance, enabling real-time alerts, lowering hospital visits, reducing caregiver stress, and supporting better long-term outcomes.
Top benefits at a glance:
- Easy to use for seniors who struggle with technology
- Higher compliance and more reliable data
- Real-time alerts for abnormal results
- Lower hospital/ER risk with early intervention
- Less caregiver burden and more peace of mind
- Better health outcomes for chronic conditions
1. Easy to Use for Seniors Who Struggle With Technology
Imagine asking an 82-year-old patient to download an app, log in, and sync a Bluetooth blood pressure monitor every morning. For many, that’s not realistic.
Cellular RPM devices like those offered by CandiHealth simplify this completely. The device itself has a built-in connection, like a cellphone, so patients only need to take the reading. The result is sent automatically to the care team.
Removing technology barriers means seniors are more likely to monitor their health consistently.
2. Higher Compliance and More Reliable Data
Consistency matters in chronic disease management. Missed blood pressure or glucose readings can hide problems until they become emergencies.With automatic data transmission, cellular RPM devices ensure readings are never forgotten or lost.
Clinics using RPM programs report higher adherence rates among elderly patients compared to traditional self-reporting methods.
3. Real-Time Alerts That Prevent Emergencies
For seniors living with conditions like heart failure or diabetes, changes can escalate quickly. A sudden weight gain or a high blood pressure spike may signal urgent risk.
As cellular RPM devices transmit readings instantly, care teams can set alerts for abnormal values. When something looks wrong, providers can call, adjust medication, or schedule an urgent visit before it becomes an ER trip.
This “early warning system” is one of the most powerful features for elderly patients, who are often more vulnerable to sudden complications.
4. Less Burden on Families and Caregivers
Caregivers often juggle reminders, logbooks, and constant check-ins: “Dad, did you check your blood pressure today?” This creates stress for both sides.
Cellular RPM removes that daily pressure. Data flows directly to providers, so families don’t have to track readings or worry about mistakes.
For caregivers, this means less emotional labor. For seniors, it means feeling more independent instead of being constantly reminded about their health.
5. A Stronger Connection Between Patients and Providers
Older adults sometimes feel isolated from their doctors between appointments. Months can pass with little contact, leaving patients unsure if anyone is keeping an eye on their health.
Cellular RPM bridges that gap. Doctors see steady updates and can reach out if something looks unusual. Patients feel supported, and that sense of connection often improves their trust in the care plan.
6. Measurable Improvements in Health Outcomes
The ultimate test is whether RPM helps patients stay healthier. Evidence says yes. Seniors in RPM programs show:
- Better control of chronic conditions like hypertension and diabetes.
- Fewer hospitalizations and ER visits.
- Higher satisfaction with their care.
For elderly patients, that translates into more independence, fewer health scares, and better quality of life at home.
RPM Challenges Solved by Cellular Devices
Even when remote patient monitoring (RPM) sounds helpful, families and clinics often hesitate. Most worries come from three big areas: technology, access, and cost. Cellular RPM devices are designed to solve each of these.
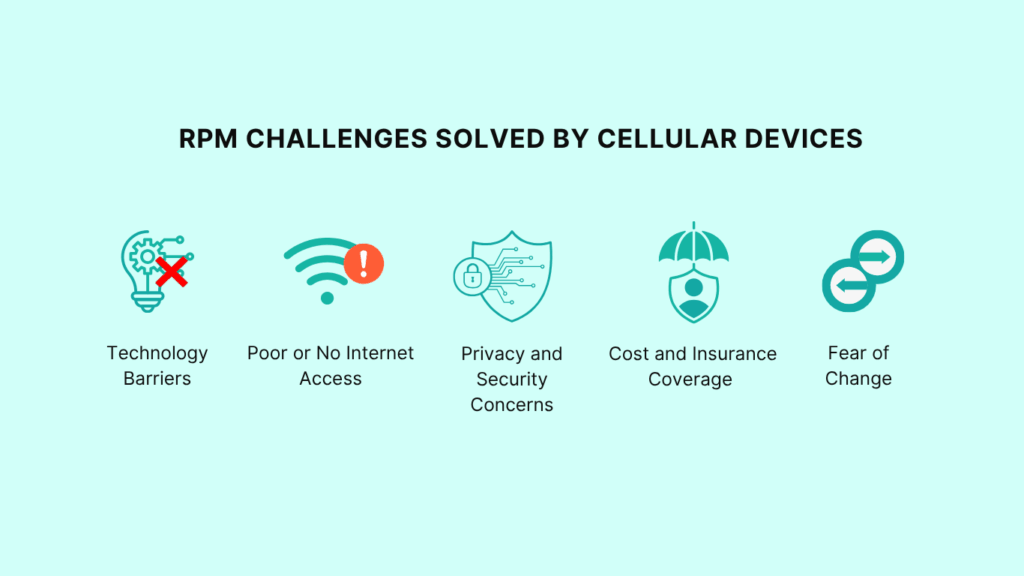
1. Technology Barriers
Many seniors aren’t comfortable with smartphones or apps. Cellular RPM devices solve this by working on their own. The device connects through a built-in signal, just like a cellphone. No Wi-Fi, passwords, or app updates are needed. Patients only need to press a button to send their data.
2. Poor or No Internet Access
A lot of older adults live in rural towns or homes with weak Wi-Fi. For them, app-based RPM is unreliable or simply doesn’t work.
Cellular devices bypass this problem. They use the same networks that power cellphones, which reach far more homes across the U.S. This means monitoring is steady, even where Wi-Fi is limited.
3. Privacy and Security Concerns
Cellular RPM devices transmit data over secure, encrypted channels. Programs that use them must follow HIPAA rules, the same laws that protect patient information in hospitals and clinics. That means the data is kept private and safe.
4. Cost and Insurance Coverage
Another concern is cost. Seniors may think new devices mean more out-of-pocket expenses.
The reality is different. Medicare covers RPM under billing codes like 99453, 99454, and 99457. This makes it easier for clinics to offer devices without placing the cost burden on patients. Families get peace of mind knowing care is affordable.
5. Fear of Change
Sometimes, the hardest challenge is not technology or money, it’s trust. Seniors may feel unsure about using a new device.
This is where cellular RPM devices shine again. Because they are so simple, many patients find them less intimidating than smartphones. With a little support at the start, most seniors quickly adapt and even feel proud of managing their health more independently.
Frequently Asked Questions on Cellular RPM Devices
1. Do cellular RPM devices really work without Wi-Fi or smartphones?
Yes. Cellular RPM devices have a built-in connection, like a cellphone. This means they can send readings to the clinic without Wi-Fi or a smartphone.
2. Which conditions can elderly patients monitor with cellular RPM?
Cellular RPM devices are often used for high blood pressure, diabetes, COPD, and heart failure. These conditions need regular tracking, and daily readings help doctors respond quickly to changes.
3. Are cellular RPM devices covered by Medicare?
Yes. Medicare covers RPM under billing codes such as 99453, 99454, 99457, and 99458. This helps keep costs low for seniors while allowing clinics to get reimbursed.
4. How safe is the data collected by RPM devices?
Data from cellular RPM devices is sent over secure, encrypted channels. Programs must follow HIPAA rules, which protect patient privacy just like hospitals do.
5. Are cellular RPM devices easy to set up for seniors living alone?
Yes. The devices are designed for simple use. Most only require the patient to press a button to take a reading. Setup is usually done by the clinic before the device is given to the patient.
6. What happens if the device loses cellular signal?
If the signal drops, the reading is stored in the device and sent once the connection returns. Patients can still use the device, and no data is lost.
7. Do families get access to the health data too, or only doctors?
By default, readings go to the care team. Some programs also share updates with family caregivers if the patient agrees. This gives families peace of mind while keeping doctors in control of treatment decisions.
8. How do cellular RPM devices improve compliance compared to Bluetooth RPM?
Cellular devices send readings automatically. Bluetooth devices often need syncing through apps, which can be hard for seniors. The simpler process leads to higher compliance rates with cellular RPM.
9. What’s the difference between cellular RPM and app-based RPM?
Cellular RPM uses built-in signals and works on its own. App-based RPM requires a smartphone and Wi-Fi to send data. Cellular devices are easier for seniors who don’t use phones or have poor internet.
10. Can rural clinics benefit from cellular RPM for elderly patients?
Yes. Cellular networks often reach rural areas better than home Wi-Fi. This makes cellular RPM especially useful for clinics serving rural seniors.
11. How much revenue can providers earn with RPM for seniors?
Providers can bill Medicare monthly for RPM services. For example, codes 99453, 99454, and 99457 can generate over $100 per patient per month. With just 50 patients, clinics may add more than $60,000 a year.
12. How do caregivers benefit from RPM programs?
Caregivers no longer have to track readings or remind patients every day. They can trust that data goes straight to the clinic. This reduces stress for families and gives seniors more independence.
13. What training do seniors need to start using cellular RPM devices?
Very little. Clinics usually show patients how to use the device once. Since most require only a button press, seniors adapt quickly. Support is also available by phone if needed.
Final Thoughts
For older adults, the hardest part of remote patient monitoring has often been the technology itself. Cellular RPM devices change that. They work without apps or Wi-Fi, making it easier for seniors to stay on track with their health.
The result is powerful: more consistent readings, faster action from doctors, fewer hospital visits, and less worry for families. Most importantly, seniors gain confidence and independence in their daily lives.
As more clinics and caregivers look for better ways to support aging patients, cellular RPM devices stand out as a simple tool with a big impact. Sometimes, the easiest solution really is the one that helps the most.