How much can you make with remote patient monitoring?
Clinics typically earn up to $100 per patient each month through RPM reimbursements. That equals about $1000 per patient per year. A practice with 100 enrolled patients can generate $90,000–$100,000 annually, while larger programs with 500 patients can reach $360,000–$460,000 per year. But it depends upon several factors that we’ll discuss later in this article.
These numbers show why RPM has become one of the most attractive revenue opportunities in healthcare. With the right setup, clinics can create steady recurring income while expanding access to care.
Let’s break it down step by step.
How Much Can You Make with Remote Patient Monitoring?
When it comes to calculating RPM earnings, there isn’t a single flat number that applies to every clinic. RPM Revenue depends on several factors such as:
- How many patients are enrolled,
- How consistently they use their devices, and
- How efficiently the practice handles billing and compliance.
What makes RPM unique compared to other services is that it creates a stream of recurring monthly reimbursements, which can be forecasted and scaled based on patient volume. To make it simple, let’s walk through six key steps that show exactly how RPM revenue is calculated.
Six Key Steps to Calculate RPM Revenue
- Understand RPM reimbursement codes
- Calculate per-patient revenue
- Scale by patient volume
- Remote patient monitoring expenses and pricing models
- Consider patient engagement and compliance
Each step covers one part of the revenue equation, from the CPT codes that drive billing to the role of patient engagement in keeping claims valid.
Step 1: Understand RPM Reimbursement Codes
The first step is to know the RPM CPT codes. These are the billing codes Medicare and private payers use to pay clinics for remote patient monitoring services. Each code covers a specific part of the service, like setup, device supply, or staff time. Here’s a clear breakdown:
| CPT Code | Description |
| 99453 | Initial setup and patient education. One-time payment, about $19–$25 per patient. |
| 99454 | Device supply and daily data transmission. Monthly payment, about $43–$47 per patient. |
| 99457 | First 20 minutes of clinical staff time reviewing data and interacting with the patient. Monthly payment, about $47–$52. |
| 99458 | Add-on for each extra 20 minutes of staff time. Around $38–$45 per add-on. |
These codes are the foundation of RPM reimbursement rates. By combining them, most clinics can bill between $80 and $120 per patient per month.
Step 2: Calculate Per-Patient Revenue
Once you know the CPT codes for remote patient monitoring, the next step is to see how much revenue one patient can generate. The numbers add up quickly when you combine setup fees with the monthly monitoring payments.
Here’s a sample calculation for a single patient:
- One-time setup (CPT 99453): $19 (average)
- Device supply & data transmission (CPT 99454): $43 per month
- Clinical staff time (CPT 99457): $47 per month
- Optional extra time (CPT 99458): $38 per month (if used)
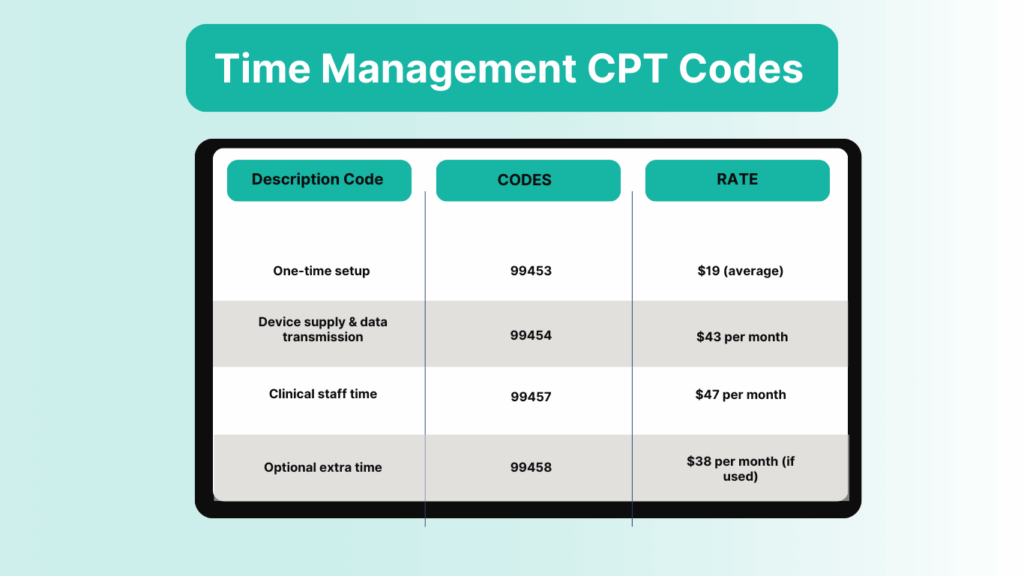
So, the average clinic earns about $100 per patient per month. Over 12 months, that comes to $1,000 per patient per year. Even if you only bill the core codes (99453, 99454, 99457), you still make around $720–$1,200 per year per patient.
This is why providers see remote patient monitoring revenue as reliable recurring income. A handful of patients won’t change much, but once you enroll 50, 100, or more, the numbers become significant.
Calculate your RPM revenue using CandiHealth free ROI calculator
Step 3: Scale by Patient Volume
The real power of remote patient monitoring comes from scaling. While one patient may bring in around $80–$100 per month on average, the numbers grow quickly when you manage dozens or hundreds of patients.
It’s important to note that CPT 99458, which pays for each additional 20 minutes of staff time, is not billed for every patient. In fact, industry data shows it applies to only about 10% of patients — usually those with complex or uncontrolled conditions who require extra attention.
This is why most clinics should calculate their RPM revenue projections using the core codes (99453, 99454, and 99457), and treat 99458 as an occasional bonus rather than a guaranteed income stream.
Here’s a realistic breakdown of RPM revenue by patient volume (based on an average of $90 per patient per month):
| Number of Patients | Monthly RPM Revenue | Annual RPM Revenue |
| 50 patients | $5,000 | $60,000 |
| 200 patients | $20,000 | $240,000 |
| 500 patients | $50,000 | $600,000 |
This table shows how quickly RPM earnings add up. Even a small primary care clinic with 50 active patients could bring in an extra $60,000 per year. A mid-sized practice with 200 patients can add nearly a quarter-million dollars, while larger groups managing 500+ patients can cross the half-million mark.
Step 4: Remote Patient Monitoring Expenses and Pricing Models
When you calculate remote patient monitoring revenue, you also need to look at the expenses. RPM is highly profitable, but costs can reduce margins if they aren’t managed carefully.
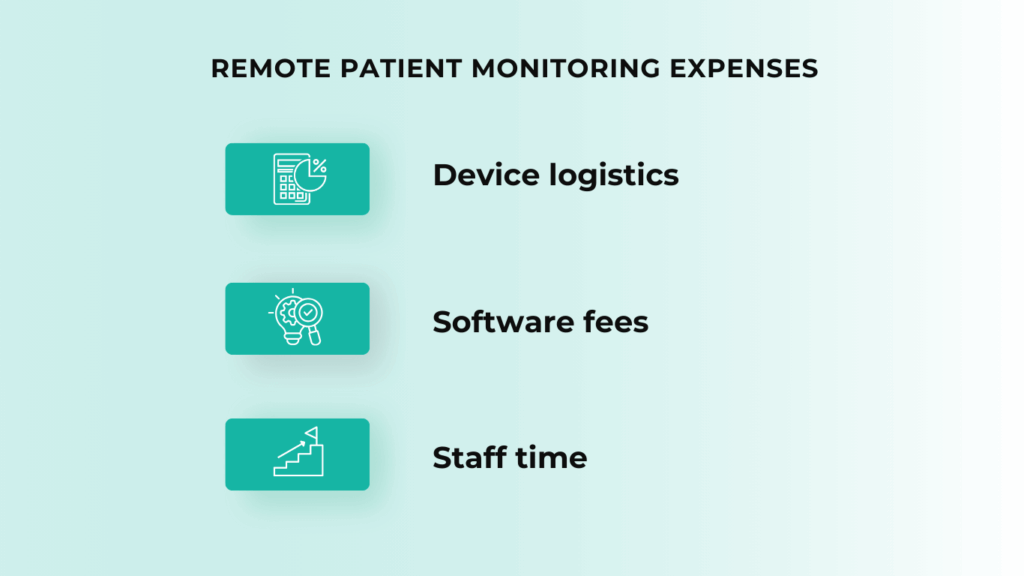
Remote Patient Monitoring Expenses
The main remote patient monitoring expenses include:
- Device logistics: Supplying blood pressure monitors, glucose meters, or other connected RPM devices. Some vendors lease devices, while others require clinics to purchase them upfront.
- Software fees: Most RPM programs run on a digital platform that collects and transmits patient data. Some vendors charge a flat monthly fee per patient, while others take a percentage of your reimbursement.
- Staff time: Nurses or medical assistants must review readings, log time, and follow up with patients. Without streamlined workflows, labor costs can climb.
Remote Patient Monitoring Pricing Model
The pricing model your vendor uses makes a huge impact on RPM profit margins:
- Revenue-sharing model: Some vendors keep 20–30% of your RPM reimbursements. This lowers your net income and can cause profits to shrink as you scale.
- Flat-fee model: Other vendors use a fixed per-patient fee. This keeps costs predictable and lets clinics retain more of their revenue.
Instead of taking a percentage, CandiHealth uses a flat $10 per-patient monthly fee. This ensures clinics maximize their RPM reimbursements without worrying about hidden costs or shrinking margins.
Step 5: Consider Patient Engagement & Compliance
Even if the billing codes and pricing models are set up correctly, the success of an RPM program depends on patient engagement. For remote patient monitoring to be billable, patients need to take regular readings and stay active in the program.
Key points about patient engagement in RPM:
- Minimum data requirements: For CPT 99454 (device supply and data transmission), most payers require at least 16 days of readings per month. If patients don’t meet this threshold, the clinic cannot bill for that month.
- Consistent participation: Patients who stop using their devices reduce revenue. High dropout rates directly affect monthly RPM reimbursements.
- Compliance tracking: Documentation is critical. If patient usage doesn’t meet compliance rules, claims can be denied.
Why this matters for RPM profit margins:
- A practice with 100 enrolled patients might only bill for 80 if engagement is low.
- Every 10% drop in compliance reduces monthly revenue by thousands of dollars.
Best practices to improve RPM compliance include:
- Educating patients during onboarding so they understand the importance of daily readings.
- Using reminders (calls, texts, or app notifications) to keep patients on track.
- Having staff check in regularly with patients who miss readings.
Clinics usually face the challenge that many patients struggle with apps, Bluetooth pairing, or Wi-Fi setup. CandiHealth solves this with cellular-enabled RPM devices that work right out of the box. Patients simply take their readings, and the data is sent automatically — no apps, no internet required. This ease of use helps boost compliance rates, which directly increases monthly reimbursements for providers.
Read: How to Increase Patient Compliance in Remote Monitoring.
Challenges That Can Reduce RPM Profitability
While the earning potential of remote patient monitoring looks impressive on paper, clinics often face obstacles that reduce their actual revenue. Understanding these challenges upfront helps providers plan better and protect their margins.
1. Device Costs and Logistics
Supplying and managing devices is one of the biggest expenses. If devices are lost, returned late, or underused, costs rise while billable reimbursements drop. Choosing cellular-ready devices can reduce technical issues that lead to patient dropouts.
2. Low Patient Engagement
If patients don’t take at least 16 readings per month, clinics cannot bill CPT 99454. Low engagement directly lowers monthly revenue. This makes patient training and support essential.
3. Billing Errors and Denials
Remote patient monitoring billing has strict documentation requirements. Missing time logs, incomplete notes, or incorrect code use can lead to claim denials. Even small mistakes repeated across multiple patients can cost clinics thousands in lost revenue.
4. Vendor Traps and Hidden Fees
Some RPM vendors charge extra fees for devices, software, or support. Others take a percentage of your reimbursement, which reduces long-term profitability. Without transparent pricing, clinics may end up with much lower margins than expected.
Expert Insight: From experience, clinics tend to do better with vendors that keep pricing straightforward and transparent. CandiHealth, for instance, uses a flat monthly fee per patient rather than taking a share of reimbursements. Many providers find this approach easier to work with because it removes uncertainty and helps them plan their budgets without the stress of hidden costs.
Final Thoughts
The real value of RPM lies in its ability to deliver both — better patient care and a steady, recurring revenue stream. Success depends on patient engagement, accurate billing, and transparent vendor partnerships.
That’s where solutions like CandiHealth can make a difference. By offering cellular-enabled devices that patients can use without apps or Wi-Fi, and a flat $10 per-patient monthly pricing model, CandiHealth helps clinics focus on outcomes while keeping revenue predictable. For providers looking to start or scale RPM, this kind of clarity and ease of use makes a program far more sustainable.
Ready to maximize your RPM revenue potential with CandiHealth? Schedule your free demo now!
Frequently Asked Questions (FAQs)
Q1. Is remote patient monitoring worth it?
Yes. Remote patient monitoring (RPM) is worth it for both clinics and patients. Clinics gain a steady stream of recurring revenue while improving care for chronic conditions like hypertension and diabetes. Patients benefit from fewer in-person visits, early detection of health issues, and closer communication with their providers.
Q2. Is remote patient monitoring profitable?
Remote patient monitoring is profitable when programs are set up correctly. On average, clinics earn $100–$120 per patient per month, which can scale into six-figure annual revenue. Profitability depends on patient engagement, accurate billing, and keeping vendor costs transparent.
Q3. How much does Medicare pay for remote patient monitoring?
Medicare reimburses RPM through specific CPT codes:
- 99453 (setup): about $19–$25 (one-time).
- 99454 (device & data): about $43–$47 monthly.
- 99457 (first 20 minutes staff time): about $47–$52 monthly.
- 99458 (extra 20 minutes): about $38–$45 monthly (applies to ~10% of patients).
In total, Medicare typically pays around $80–$100 per patient per month on average.
Q4. How much does remote patient monitoring cost?
The cost of RPM depends on the vendor pricing model. Some vendors take a percentage of reimbursements (20–30%), which lowers profits. Others charge a flat monthly fee per patient. For example, models like CandiHealth’s $10 flat fee keep costs predictable, allowing clinics to keep more of their revenue. In most cases, clinics retain 70–80% of reimbursements as profit after covering device, software, and staff costs.