Table of Contents
Hypertension remains one of the most widespread health issues globally. According to the World Health Organization, over 1.28 billion adults aged 30–79 suffer from high blood pressure. These numbers underscore a persistent challenge in managing hypertension long-term.
In most cases, blood pressure is checked during clinic visits that happen weeks or months apart. These occasional readings don’t reflect the daily fluctuations caused by stress, activity, meals, or medication timing. As a result, important changes often go unnoticed.
Managing hypertension requires consistent monitoring, timely intervention, and ongoing lifestyle changes. However, traditional care models fall short in tracking patients outside the clinic. This is where Remote Patient Monitoring (RPM) makes the difference.
This blog explains how RPM helps providers manage hypertension effectively, improve outcomes, and reduce long-term healthcare costs.
What Is Remote Patient Monitoring and Why It Matters for Hypertension
Remote Patient Monitoring is a technology-enabled care approach where patients use connected devices at home to track health metrics. These devices automatically transmit data, such as blood pressure readings, to healthcare providers in real time or at regular intervals. RPM platforms typically include:
- A blood pressure monitor with cellular or Bluetooth capability
- A cloud-based dashboard for healthcare providers
RPM enables providers to monitor patients daily without requiring in-person visits. It shifts hypertension care from episodic check-ins to continuous management.
How RPM Works for Hypertension
- The clinic provides a pre-configured blood pressure monitor.
- The patient uses it from home—no smartphone or Wi-Fi needed.
- Readings are sent automatically to the provider’s dashboard.
- Care teams receive alerts if readings fall outside the safe range.
- Clinicians follow up directly with the patient, if needed.
Unlike traditional care models, RPM doesn’t depend on the patient initiating contact. The system runs in the background, capturing consistent data and making early intervention possible.
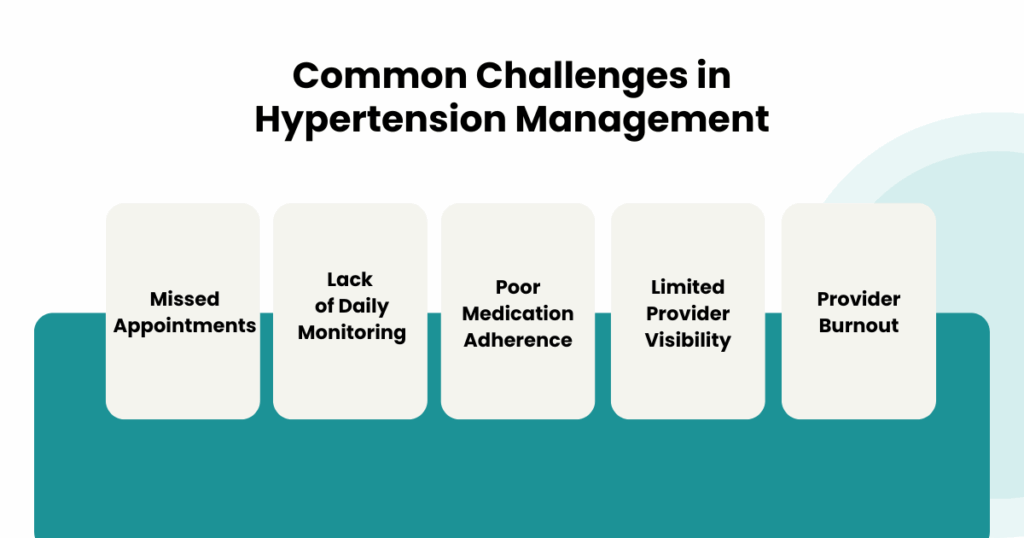
Common Challenges in Hypertension Management
Despite medical advancements, many patients with hypertension remain uncontrolled. The reasons are practical, not clinical:
1. Missed Appointments
Patients often skip routine visits due to transportation issues, cost, or lack of symptoms.
2. Lack of Daily Monitoring
Office readings offer only a snapshot. Blood pressure fluctuates throughout the day, and a single reading doesn’t reflect overall control.
3. Poor Medication Adherence
Many patients stop taking medication due to side effects, costs, or forgetfulness. Providers often discover this too late.
4. Limited Provider Visibility
Without daily data, providers rely on patient memory or outdated logs. This makes timely treatment adjustments difficult.
5. Provider Burnout
Physicians already manage heavy caseloads. Calling patients, tracking spreadsheets, or chasing follow-ups strains resources further.
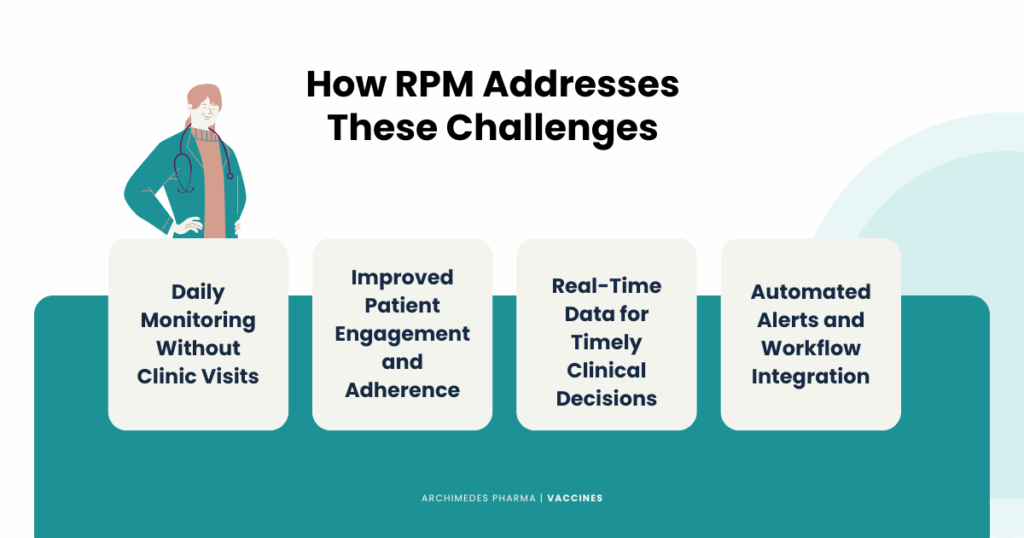
How RPM Addresses These Challenges
Remote Patient Monitoring solves these issues with a structured and scalable approach to care.
1. Daily Monitoring Without Clinic Visits
Patients take their blood pressure at home using a pre-configured device. The data uploads automatically to the provider dashboard. No manual entry. No app setup. No travel.
This ensures consistent readings that reflect timely blood pressure trends—not just occasional check-ups.
2. Improved Patient Engagement and Adherence
RPM empowers patients to take control. Many platforms include reminders, visual graphs, and educational content. Patients see their progress and understand when action is needed.
Knowing that a care team is watching also increases accountability. Patients are more likely to follow their medication plans and report issues early.
3. Real-Time Data for Timely Clinical Decisions
With RPM, providers can see exact patterns, identify morning surges or nighttime spikes, and adjust treatment before complications occur.
Clinical staff receive alerts when readings cross a defined threshold. They can call the patient, modify medication, or schedule a visit proactively.
4. Automated Alerts and Workflow Integration
RPM systems automatically highlight abnormal readings. Triage protocols help staff decide when and how to respond. This saves time and ensures no patient slips through the cracks.
Most platforms also integrate with Electronic Health Records (EHR), so all RPM data becomes part of the patient’s official chart. This supports better care coordination across teams.
Clinical Evidence Supporting RPM for Hypertension
Several studies confirm the clinical value of RPM in managing hypertension.
1. Large-Scale Cohort Study (Cells/Cellular RPM Devices)
A meta-analysis published in Hypertension found that patients using RPM with clinical support had a significant reduction in systolic and diastolic blood pressure compared to those receiving standard care.
- Average systolic BP fell from 135 mmHg to 127.8 mmHg (↓7.3 mmHg), while stage 2 hypertension patients improved by 16.7 mmHg.
- The proportion of uncontrolled hypertension decreased from 66.3% to 40.2% (p < 0.01)
Source: PMC, Remote Patient Monitoring Is Associated with Improved Outcomes
2. RPM with Nurse‑Led Care Coaching (Stage 2 Hypertension)
In 2025, the American Journal of Managed Care published a retrospective cohort of 1,594 participating Medicare patients with stage 2 hypertension (652 patients):
- Mean SBP/DBP dropped from 152/85 to 132/74 mmHg by 12 months
- Stage 2 hypertension rates fell from 100% to 25%
Source: AJMC, “Effect of Remote Patient Monitoring on Stage 2 Hypertension”
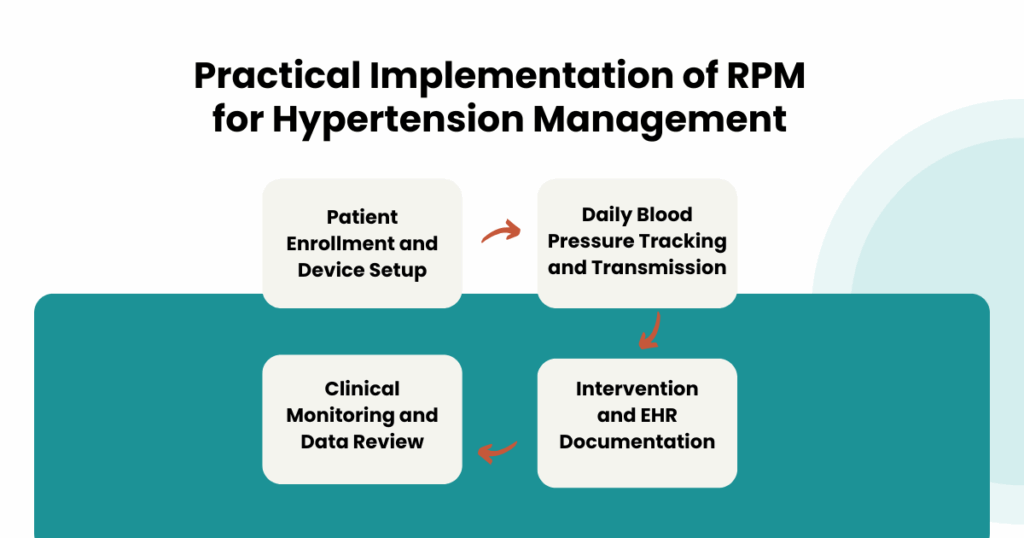
What RPM Looks Like in Practice
Let’s walk through a typical RPM experience for a hypertension patient.
Step 1: Enrollment
The clinic identifies a patient with uncontrolled blood pressure. The provider prescribes RPM and gives the patient a cellular blood pressure cuff. No app installation or setup is needed.
Step 2: Daily Use
The patient takes their blood pressure once or twice a day. The device sends data to the clinic dashboard automatically.
Step 3: Monitoring
The clinical staff reviews the readings during routine checks or receives alerts if values fall outside preset ranges.
Step 4: Intervention and Documentation
If a pattern shows rising blood pressure, a nurse calls the patient. They may check for missed medication, dietary habits, or stress. The doctor can adjust medication if needed. All readings and interventions are documented in the EHR for billing and compliance.
This approach keeps both the patient and provider informed, reduces guesswork, and improves control rates.
Conclusion
Remote Patient Monitoring provides a reliable, efficient, and scalable way to manage hypertension. It brings visibility to daily blood pressure trends, supports early intervention, and reduces the burden on both patients and providers.
Healthcare providers who integrate RPM into their hypertension management strategy stand to improve clinical performance, reduce hospitalizations, and meet the growing demand for remote care.
CandiHealth’s RPM platform is built to support exactly this kind of care—simple to deploy, compliant with CMS, and fully tailored for chronic conditions like hypertension.
If you’re a provider looking to start or scale your RPM program, get in touch with us to explore how CandiHealth can help streamline your hypertension care and improve patient outcomes.
Related Articles
What is Remote Patient Monitoring (RPM) and How It’s Transforming Chronic Care
Benefits of Remote Patient Monitoring for Patients and Providers
Frequently Asked Questions (FAQs)
Can remote patient monitoring be an effective way to monitor patients with hypertension?
Yes, remote patient monitoring (RPM) is an effective approach for managing hypertension. It allows patients to record and transmit daily blood pressure readings from home, giving providers consistent and accurate data. This real-time visibility supports early intervention, timely medication adjustments, and improved long-term blood pressure control.
2. How can we effectively manage or reduce hypertension?
Effective hypertension management includes a combination of lifestyle changes, medication adherence, and consistent monitoring. Remote patient monitoring supports this by ensuring daily tracking, enabling personalized care plans, and improving patient engagement
3. What are the benefits of remote blood pressure monitoring?
Remote blood pressure monitoring provides several benefits:
- Continuous tracking outside clinic visits
- Early detection of rising trends
- Improved medication adherence
- Reduced clinic visits and hospitalizations
- Better communication between patient and provider
4. How effective is remote patient monitoring?
Clinical studies show that RPM significantly improves blood pressure control. Patients using RPM are more likely to achieve target blood pressure levels and maintain consistent adherence to care plans. It also helps providers intervene early, reducing the risk of complications and hospital admissions.